Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
Although the US exceeded 700,000 COVID deaths this week, new cases have fallen 25% over the last 2 weeks. We are likely on the downside of the current surge. Locally, we had a decrease in the number of people we diagnosed with Covid in the emergency department this week. Each time I order a Covid test, I am required to document if the patient is “symptomatic” or “asymptomatic.” There are clinical guidelines that we follow that define each of those though there is also a certain amount of subjectivity on the ordering physician side. After about 18 months of doing these tests, I like to believe that most people are fairly consistent in the box that they check. We generally check about 90-100 patients a week who we classified as symptomatic. Our positivity rates have been as high as 40 to 50% during the first surge as well as the surgery saw last winter. Over the summer months are positivity rates were generally in the single digits. Since late July, this number has generally ranged between 15 and 20%. We typically see positive cases every day and having a day where we did not have any positive cases among the symptomatic patient population would be highly unusual. With that said, we went 2 days in a row this past week without any positive cases. Our percent positive rate among symptomatic patients for the past week was almost 25% below our 6-week running average. Our percent positive rate among our asymptomatic patients was also a bit down compared to last week but still higher than our 6-week running average. Last week I reported a pretty significant increase in the amount of positive cases among all comers to the emergency department. This week, it did fall off some and is more consistent with the 6-week average.
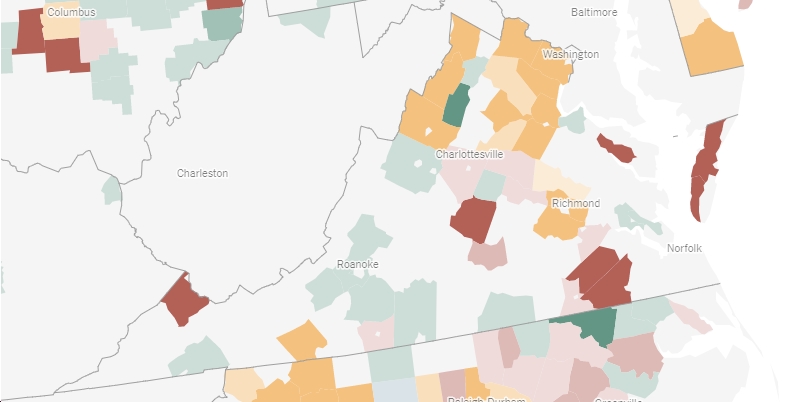
Our hospital census is also down a bit compared to last week. You may recall that we saw a jump last week and while it’s not retreated to the levels it’s been the last 6 weeks, it’s lower than last week. We also saw a drop in the number of patients requiring COVID isolation and a decline in the number of patients admitted from this population. There are some other hospitals around the state that still have a very heavy burden of COVID patients, but Northern Virginia appears to be doing better.
The CDC issued a statement on the impact of COVID in the pregnant woman. Only about 32% of pregnant women are vaccinated. Pregnant women with develop COVID are at “increased risk of adverse pregnancy outcomes that could include preterm birth, stillbirth, and admission into the ICU of a newborn also infected with COVID-19.” Pregnant women with COVID are two times more likely to get admitted to the ICU and 70% more likely to die compared to non-pregnant women. All of this together has led the CDC to “strongly recommend” vaccination for pregnant women or those thinking about getting pregnant. The added bonus is that the baby gets protection when born as well.
The CDC released 3 studies looking at the impact of COVID case rates between school systems that mandates masking versus those that did not have mandates in place. No one should really be surprised by the findings but the CDC said, “Nationwide, counties without masking requirements saw the number of pediatric COVID-19 cases increase nearly twice as quickly during this same period.” In a study from Arizona, “two of the state’s most populous counties were 3.5 times more likely to have COVID-19 outbreaks if they did not have a mask requirement at the start of school compared with schools that required universal masking on day one.” New case rates were also lower in school districts that mandated masking compared to those that didn’t. Masks definitely seem to work. The third paper showed that despite school closures and case spread, 96% of public schools have been able to remain open for full in person learning so far this year.
Something to keep an eye on: Merck released a press statement about a new oral antiviral medication called Molnupiravir to treat COVID in the outpatient setting. This phase 3 trial looked at 762 patients who had mild to moderate COVID, at least one risk factor, onset of symptoms 5 days or less, and did not require hospitalization. At day 29, there was a 50% reduction in hospitalization and/or death for those who received treatment. No deaths were reported among the 385 patients who received Molnupiravir compared to 8 deaths in the placebo group. The drug also appeared effective against the current worrisome variants. Merck will be applying for emergency use authorization and it will certainly be interesting to get a better look at the data. Certainly, it looks like a promising treatment though it has the potential to exacerbate health equity issues because of access to care (symptoms 5 days or less) and cost (potentially $700). More to come.
On an ER and vaccine note, but not related to COVID, Illinois reported its human first rabies death in 70 years. We regularly see patients with possible rabies exposure in the ER. Unfortunately, exposures and/or bites from bats, raccoons, feral cats, and even some dogs (that can’t be tracked) lead people to the ER We generally work with the health department to determine risk and appropriateness of giving rabies vaccine. Because rabies is universally fatal if untreated, our threshold to offer/give vaccine is appropriately fairly low. I once took care of a family of 6 who had been playing with feral kittens who ultimately had rabies, after exposing the whole family. There are some basic rules. Because bats are known to be carriers, if you wake up to find a bat in your bedroom, you need vaccine. Bats have very small teeth and can bite you while you’re asleep without you realizing it. The first time I found a bat in my house, I swore I’d move if it happened again. 15 years later, there was another bat. This one was caught and sent to the health department. I learned a lot during that experience. At the time, about 5% of bats in my county were testing positive for rabies, which was lower than I expected. This bat did not have rabies and we didn’t need to vaccinated. (We also came home to find the bat in the house and don’t believe it was there when we were asleep but we did have some stressful conversation with the health department) So let’s get back to the Illinois man. (No HIPAA issues as the case was well reported in the news) 87 year old guy bit by a bat that tested positive for rabies. He refused the rabies vaccine series. About a month later, he started to experience symptoms consistent with rabies—neck pain, headache, numbness, and other neurologic symptoms. He ultimately died. Rabies is very rare in America. But rabies exposure is common. About 60,000 people annually receive post exposure treatment each year. The vaccination series is pretty easy. The first day is usually a couple of shots then the patient returns on days 3, 7, and 14 (you used to return on day 28 as well but that stopped a few years ago) for one shot each visit. You used to be able to get follow up vaccine at the pharmacy but then a national shortage about 15 years ago led to the need to return to a hospital. The follow up visits are usually pretty quick. The overall treatment is quite expensive, but without treatment, the virus infects the nervous system and is generally fatal.
Earlier this week, VHC held our first ever Trauma Survivor Day. (shout out to my nursing leadership partner Taryn who did an amazing job organizing this). There were a few speeches from our team. I gave a short speech about the importance of teamwork in the ER and the care of the trauma patient. The best part of the day was the speech by the patient and his parents. Over 100 people were involved in this patient’s care—from docs, advanced practice providers, nurses, techs, lab and radiology personnel, food services, etc…The speeches by the family were heartwarming and helped to remind everyone in the audience the positive outcomes we contribute to. So often, as clinicians we are focused on the next patient or task or we only remember the bad outcomes, the difficult patients, or the ones who complain, we forget to take the wins when we can. The last 18 months have been really rough, so although I went into this event as just an hour on my calendar, it really was an important part of my week.
Science matters. Get vaccinated. Wear a mask. We’re not quite there.
Mike