Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
Friday Night Update from the ER in Arlington, VA
Pediatric illnesses have been in the news a lot this week. During my last shift, I had kids infected with COVID, influenza, and RSV. By far, the sickest of the three was the one with RSV. Respiratory syncytial virus (RSV) is a fairly common virus that causes something called bronchiolitis. This is a respiratory tract infection that can cause coughing, shortness of breath, and a low oxygen level. It impacts kids less than 2 much harder than the kids who are older. It is also possible to get as an adult though we typically stop testing for long before a child is a teenager. We’re seeing a lot more cases of RSV then we typically see this time of year. While only a fraction of kids who have RSV require hospitalization, we are already seeing pediatric intensive care units (PICU) in the area reach critical occupancy levels.
Unfortunately, this means that some kids who would normally be placed in a PICU may spend additional time in the emergency department waiting for a bed to become available. Additionally, there may be additional time a patient spends in another hospital’s ER waiting to be transferred to one of the handful of hospitals in the DMV that have PICU beds, from whichever emergency department the patient was initially seen in. It also means that some patients who are borderline and might often get a PICU bed versus a hospital floor bed, may not get the PICU bed because beds are prioritized to sicker patients. (We saw all of this with COVID during our big surges, just in the adult population).
I talked to a friend yesterday who works at another emergency department, and that ER had an intubated child in their emergency department for about 24 hours. This was a hospital without a pediatric intensive care doctor, or even a pediatrician, who could assist with the patient’s care. Unfortunately, I am concerned that this will be the new norm for critically ill pediatric patients for the next 3 to 5 months.
Of course, there is a trickle-down effect to this as well. Anytime we have patients boarding in the emergency department, (boarders are broadly defined as patients who require hospitalization but the hospital doesn’t have space for them at the moment so they stay in the ER and get their care), we then have beds that are not available to be used for the new patients that are arriving to the emergency department. Now add in that critical care patients that are boarding require much more nursing involvement, and now those nurses are not available to take care of other emergency department patients.
These younger children have only been alive during the pandemic. For the most part, they have not had the normal exposure to viruses that kids got prior to the pandemic. It’s not that their immune system is weak, rather they are naïve to routine viruses. There is clearly still a role for good hand hygiene and mask wearing (and of course routine vaccinations) as we move forward in our COVID world.
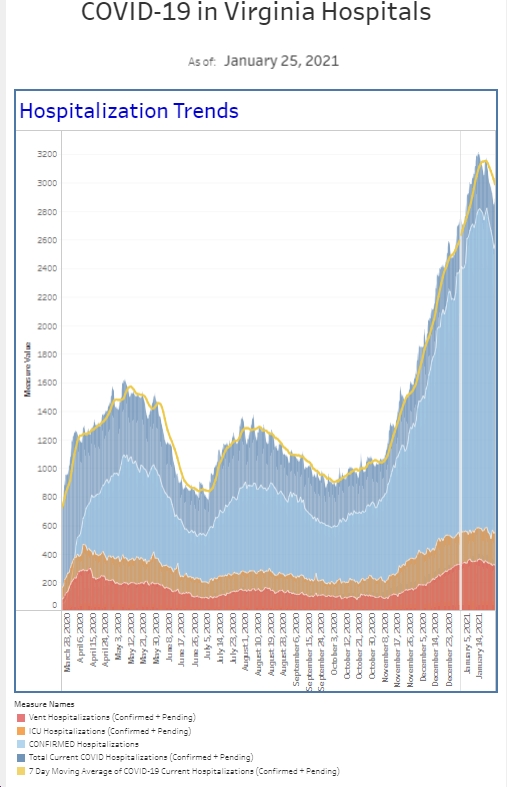
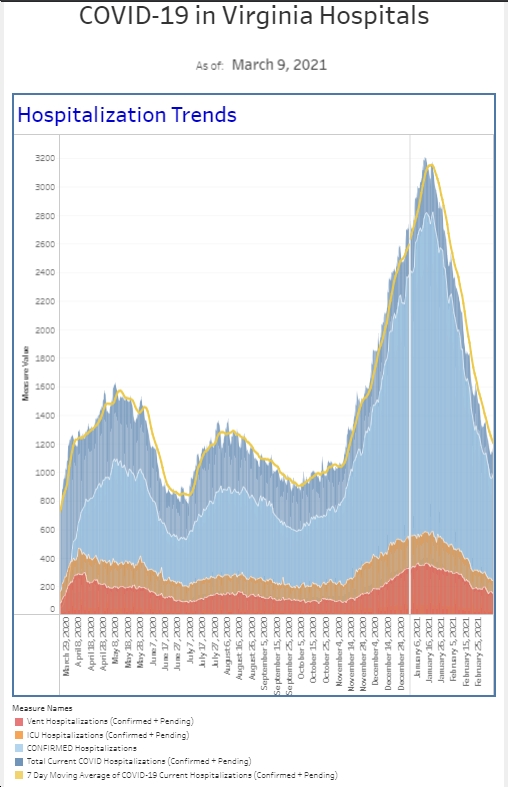
On the positive side, the [number] of people hospitalized with COVID currently is below last week. The number of patients that we diagnosed with COVID in the emergency department this past week is also a touch below previous week (and the percent positivity is down a touch as well).
Coronavirus is not quite done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike