Thanks to Dr. Mike Silverman (Chair, Department of Emergency medicine at Virginia Hospital Center) for his latest “Friday Night Update from the ER in Arlington, VA”; these are very helpful!
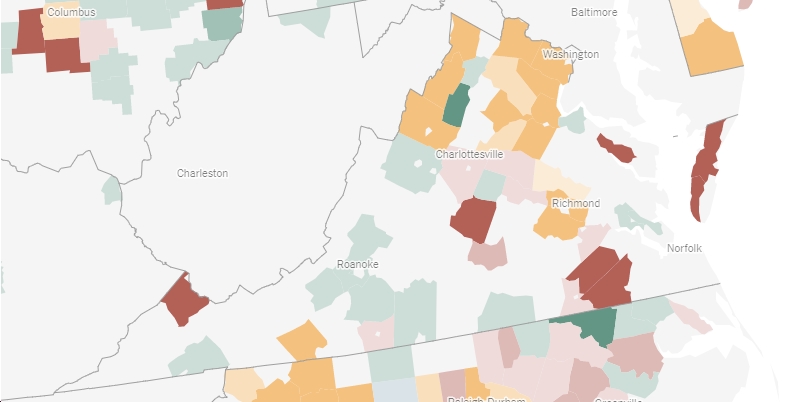
Virginia is at an 7% positivity rate. Arlington County around 4%. 5% has always been defined as the key threshold by public health officials to consider additional restrictions or mitigation factors. I was asked this week if I think we’re going to have another lockdown. I don’t want a lockdown nor do I think we are headed back there but I do believe we can’t “hope” we improve. Vaccination and indoor masking are the best actions we can do as a society. I’m glad to see vaccinations numbers increasing and appreciate anytime someone asks me a question about it.
We continue to see gradual increases in our numbers in both the ER and the hospital census with COVID patients. We are still far from surge peaks but over the last 4 weeks, we are definitely seeing a gradual and consistent increase. We tested a lot more “symptomatic” patients in the ER this week and had the largest amount of positives we’ve seen in some time. Our total number of positives and our positivity rate are also climbing in the ER. I’m hearing from our hospitalist team that most of our hospitalizations are in unvaccinated patients. For the ones who are vaccinated, they believe there is a higher proportion of patients who had J&J and international patients who received AstraZeneca but this is not based on objective data. I am hearing that the vaccinated patients tend to be less ill. Unfortunately, we’re starting to see some vaccinated employees test positive as well. In a review of recent positive case data, our team believes that about 25% of our positive tests across the whole hospital system are among vaccinated patients.
The CDC report from July 30th reviewing the outbreak in Massachusetts almost seems like old news at this point. But there are some critical points. Briefly, over a 2 week period in Barnstable County, MA (Cape Cod), there were 469 Massachusetts residents who tested positive for COVID after traveling to that region. 133 of these patients had testing genomic sequencing performed, and 90% had the Delta Variant. (Nationally, CDC is estimating Delta makes up more than 93% of new cases). About 74% of cases occurred in fully vaccinated patients. 79% of patients were symptomatic. Five patients required hospitalization, 4 of which were vaccinated. Fortunately, no deaths were reported. Viral load levels were determined to be similar (via RT-PCR cycle thresholds) between vaccinated and unvaccinated patients. This review showed three things. First, Delta is the dominant variant. Second, it’s highly transmissible even if you’ve been vaccinated. Third, vaccinated people have viral loads that makes them more contagious compared to other variants. Taken together, this data formed the recommendation for indoor mask wearing based on the prevalence of COVID in your local area. This is a rapid public health review and recommendation and why we’ve been saying the Delta variant is a game changer for the last month.
One of the questions I hear a lot is “why should I get vaccinated if I can still get COVID and I need to wear a mask?” It’s a fair question. While we don’t know the exact efficacy of the vaccine on preventing illness, we know it does reduce the risk of getting COVID. Recall, last week I compared data out of the UK and Israel on the efficacy of the vaccine and the numbers were pretty different (though still better than being unvaccinated). There is a pre-print, not yet peer reviewed paper from the Imperial College London’s “Real-time Assessment of Community Transmission,” or REACT-1, which is an ongoing coronavirus monitoring study, that came out 2 days ago looking at 100,000 people who did at home tests between June 24th and July 12th. There looks to be a 50-60% reduction in getting COVID compared to unvaccinated patients. Breaking the data down a bit more, it showed people are 49% less likely to be asymptomatic and 60% less likely to be symptomatic compared to unvaccinated patients. All of the positive cases that underwent genomic sequencing were the Delta variant. That’s reason number one to get vaccinated. It still prevents you from getting sick and spreading the disease compared to unvaccinated people. Reason number two is that vaccinated patients are hugely protected from severe illness and death. Nationally, unvaccinated patients still make up about 98% of hospitalized patients and deaths. Even if you’re vaccinated, masks are still an easy mitigation strategy to protect you from getting and/or spreading COVID. Indoor mask use improves your chances of not getting COVID if you’re exposed and will help reduce your spread if you are contagious.
In a recently published study in the NEJM on Regeneron (a monoclonal antibody, MAB), it appears that there is a role for post exposure prophylaxis for those at high risk of not mounting an immune response after a household contact. (i.e,. a transplant patient whose spouse tests positive for COVID and exposure has occurred). This study suggests that the MAB can help reduce the risk of the individual getting COVID by more than 80%. Potential patients include anyone who is immunosuppressed (disease) or on immunosuppressive medications who have had a COVID exposure. It is actually tricky to identify the right patients and I can foresee significant challenges getting it administered (where is the right environment and can PCP’s or transplant teams arrange this for their patients). But it’s certainly a potential way to keep vulnerable patients healthy.
Only 16% of pregnant women are vaccinated according to a June CDC report though “tens of thousands of pregnant women” have been vaccinated. And this is despite evidence that having COVID during pregnancy increases the risk of severe disease and death. The American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) have come together to “strongly recommend” that all pregnant women get the COVID vaccine. These are the two leading national physician groups that care for pregnant women and recommendations like this are made after review of data and discussion by leaders about the risks and benefits.
Because the vaccine offers out best solution to returning life to normal, the FDA has entered a “sprint” to reach a decision about granting full approval to the Pfizer vaccine. This involves accelerating data review and meetings. The hope is that full approval will add a layer of comfort to vaccine hesitant people and will likely increase the number of businesses, including hospitals, in mandating employee vaccination. I hear rumors of a Labor Day target, but I will believe it when I see it. I also hope the data continues to roll in regarding the benefit and/or need for a booster shot and we get a better understanding of what that timing looks like. (I’m hearing rumors of late September).
Science matters. Get vaccinated. Wear a mask when you’re supposed to. We’re almost there.
Mike