Another helpful update from Dr. Mike Silverman, Chair, Department of Emergency medicine at Virginia Hospital Center. Thanks!
Friday Night Update from the ER in Arlington, VA
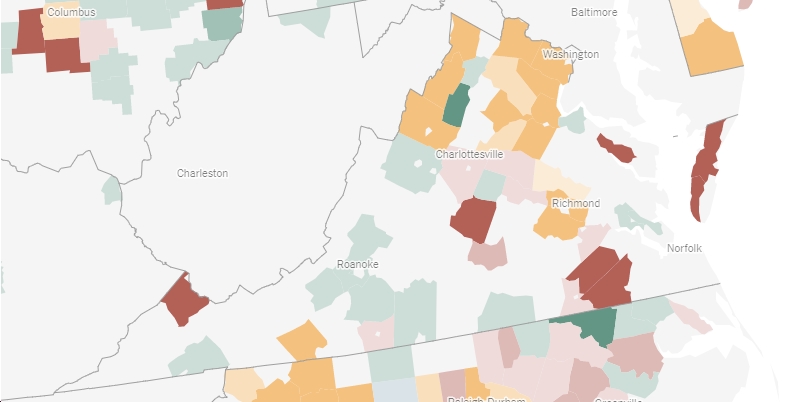
Although last Friday I reported that our number of Covid patients had declined compared to the previous week, unfortunately this week I must report that our numbers rebounded and increased to a level we have not seen since early March. We saw increases in the number of patients we diagnosed with Covid among our symptomatic and our asymptomatic categories. We also saw increases in the percent positive rate of all patients that we tested. Our hospitalized patient numbers have also increased from last week. At one point this week, we were about 50% over last week’s total but things leveled off and it’s not that dramatic as of this morning.
Let’s follow-up on some old business from last week. I said that my daughter got her flu shot before she left for college. Flu shots are now available in most pharmacies so it’s important to make a plan to get your flu shot. There are 2 timing issues to consider. First, you want to make sure you get it a couple weeks before flu starts to show up in the area. The flu vaccine will provide protection for about 6 months, so if you get it in late summer and then our flu season does not peak until March, you may put yourself at some unnecessary risk. I get my flu shot either at the national meeting of emergency medicine physicians that typically occurs in late September or early October, or I get it through the hospital which typically provides vaccination for staff in the same timeframe. If these opportunities occurred earlier in September or later in October, I would get my flu shot then as well. Definitely get your flu shot by the end of October. Flu season is generally in the winter and I have not had the flu in more than 20 years since I started getting the vaccine.
The other potential timing issue is how it interacts with the Covid booster. In theory, I will get my booster the week of September 20. When Covid first appeared last winter, the CDC recommended not getting the vaccine within 14 days of any other immunizations. This was precautionary, as the CDC has written, it was done “out of an abundance of caution and not due to any known safety or immunogenicity concerns.” As with many things Covid, recommendations change over time as we learn more about each aspect of care and the disease. The CDC is now able to revise their guidelines because “substantial data have now been collected regarding the safety of COVID-19 vaccines.” Although guidelines may change again, the current recommendations are that it is okay to co-administer the Covid vaccine with other vaccines. No longer is there a recommended 14-day window between the two vaccines. My guess is I will get them both around the same time. I’m not exactly sure of how the hospital will handle booster shots and flu shots yet. But I’m not worried about it.
I also had a lot of questions about monoclonal antibodies (MAB). There is no doubt that there is a role for this therapy for certain patients, but this treatment modality is not meant to be used for everyone who has Covid. Just like remdesivir and steroids are used in hospitalized patients that require oxygen, monoclonal antibodies are used as outpatient therapy for high-risk patients. MAB were initially introduced to provide immunity to those who didn’t have antibodies—prior to the vaccination and for those who hadn’t had COVID initially. In theory, if you’re vaccinated, your body has developed antibodies and you shouldn’t need MAB therapy. Initially, we thought we would need to treat about 20 patients with MAB to prevent one hospitalization and/or death. With the Delta variant, it’s unclear what the NNT is now, though it’s believed to be higher than it was because there are vaccinated patients getting COVID. Again, if you’re vaccinated, you have the antibodies.
Patient selection for this therapy again is based on the high risk patient criteria, and now could include a small subset of vaccinated patients who are immunosuppressed and are eligible for a booster. In the outpatient setting, it can be very challenging for patients to find a way to get the monoclonal antibody therapy. In a perfect world, primary care doctors should be able to coordinate this but for variety of reasons, I have found this to be inconsistent. As an ER doc, I have a love-hate (said with heavy sarcasm) relationship with his therapy. I love that it will likely keep some people out of the emergency department, preventing hospitalization and death. On the other hand, the ER is generally not the right setting for patients to receive this treatment as it takes two plus hours to thaw the MAB, administer the treatment, and monitor the patient for an allergic reaction after administration. Right now, that bed space and nursing time is better used for higher priority patients. Additionally, the therapy can be given within 10 days of onset of symptoms, so many patients discharged from the emergency department still have time to get it done as an outpatient.
However, it can be very challenging for patients to get it arranged as an outpatient. Our doctors at VHC, can prescribe it and have it done in the outpatient setting. Other hospitals in the area have set up clinics as well, but my sense is that it’s still not as accessible as it should be for all the patients who may benefit from it. The best thing you can do for yourself to prevent hospitalization and death is to get vaccinated. Then your body is making the antibodies and you don’t need to rely on the monoclonal antibodies (generally speaking). And soon enough, many people will be able to get the booster shot to supercharge your own antibody response.
Keeping in mind that the goal of MAB is to reduce the risk of hospitalization and death, the CDC released data this week showing the vaccines to be “extremely effective” in preventing hospitalizations against the Delta variant. Over the last couple of months when the Delta variant has prevailed, the vaccine efficacy against hospitalization has ranged from 75-95%. Looking at age ranges, it’s probably about 80% effective for those over 75 years old and 94% effective for those 18-49 years old. In fact, unvaccinated adults were 17 times more likely to be hospitalized than vaccinated adults. The best thing we can do to fight COVID is to continue to get everyone eligible vaccinated.
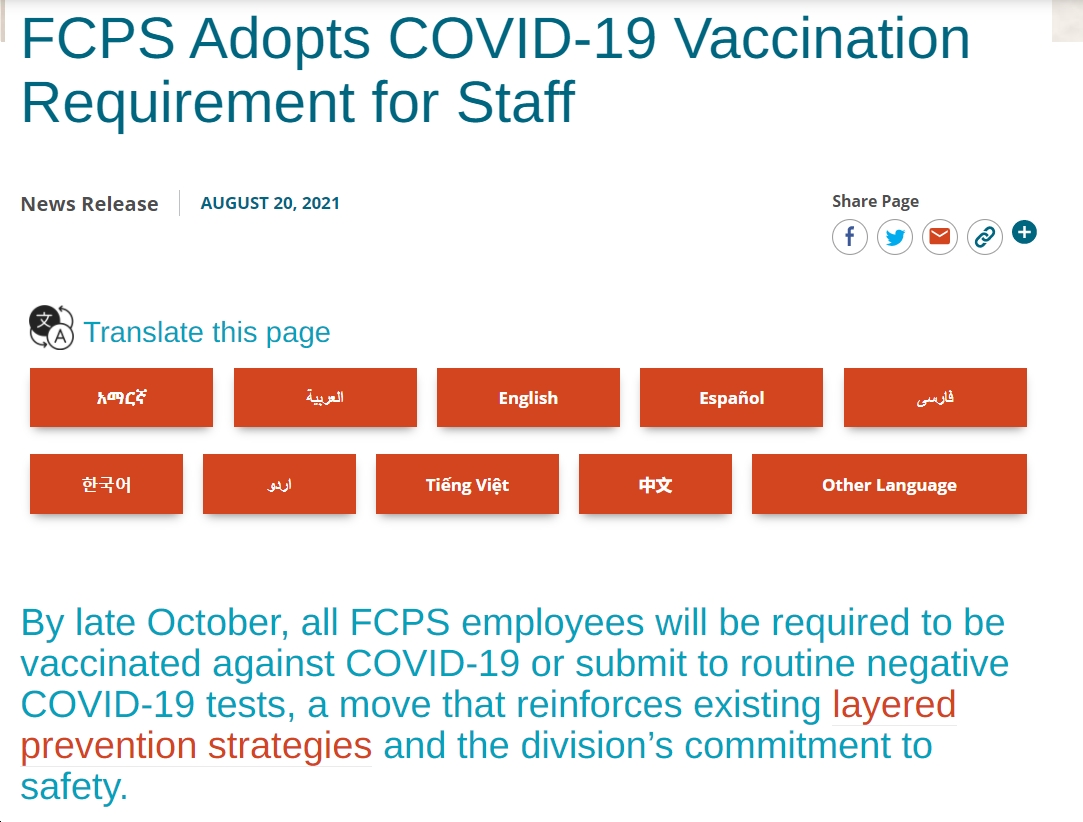
As I just alluded to, ER’s are crowded. We’re seeing this in the DMV, not just in the south. Essentially, every ER colleague I talk to in the area is telling me they’re very busy with very sick patients. Although COVID is a part of this, it’s not the only reason as our COVID volume is generally less than half of what it was during the winter surge. Although ER volumes significantly declined early in the pandemic, they’ve been coming back for months. Most people I speak with are back to not only “normal” or higher volumes than pre-pandemic, but we’re now also taking care of sicker patients, which take more time and resources. It’s unclear as to the exact cause of this. It’s likely that people put off preventative healthcare and our now dealing with complications of that. For example, we’re seeing more patients with elevated blood sugars. We’re also seeing more trauma, more substance abuse, and more psychiatric patients. We’re all feeling the stress of the pandemic. I will tell you that doctors, nurses, and others who work in hospitals are tired. I’ve seen a lot of people leave hospital-based jobs. I know a lot of people of are “done with” COVID and want to go back to their normal lives. I’m also very tired of COVID. But it’s not done with us. It’s possible cases are peaking in the south but that doesn’t mean we won’t have high numbers of infections for the next several weeks. I share the stress that many parents feel whose kids are back in school and not vaccinated. We’ll certainly need to keep a close eye on pediatric infections in the area going forward.
I have a few things to close out with regarding Israel, Moderna, and new variants. Israel led the world in early mass vaccinations. They’re now seeing a spike in cases, likely due to waning immunity. They’re also giving boosters to everyone 12 and older. A recent study shows that a Pfizer booster may increase protection 11-13 times by day 16, perhaps making it 92% effective against infection and 94% against severe disease. Moderna data is likely to be even better. A recent study out of Belgium found that healthcare workers had 2.6 times higher antibody levels if they received Moderna rather than Pfizer.
There are two new variants to follow. The first is Mu. It was first identified in Columbia and Ecuador, is found in dozens of countries, and there are a sprinkling of cases around America, though at least a handful of cases in nearly every state. It is possible that the mutations in Mu have the “potential to evade immunity.” Another variant that has been in the press, is known as C.1.2 and is being reported on in South Africa, based on a pre-print article out of their NIH (remember pre-print is not yet peer reviewed). This variant has mutated the most from the original strain, so there is also some concern it could evade the vaccine. It’s also mutating faster than other variants which means it’s likely to give rise to additional variants. C1.2 has increased in frequency among sequenced cases in S. Africa, going from 0.2% in May to 1.6% in June to 3% in July. This pattern is reminiscent to Delta. (Delta is currently 87% of cases in S. Africa) We don’t know if either variant is more contagious, more dangerous, and really, what will happen with either variant, but both are worth some awareness.
My daughter was supposed to go to a large outdoor music festival this weekend. I had my concerns but didn’t discuss them with her. She and her friends made the decision to skip it. In their opinion, it wasn’t worth the risk to be partying in a mass gathering.
We all want our normal life back, but COVID is not done with us.
Science matters. Get vaccinated. Wear a mask. We’re not quite there.
Mike