Thanks as always to Dr. Mike Silverman, Chair of the epartment of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
As a hospital, we crossed a pretty big COVID milestone recently. We’ve now taken care of over 2,000 COVID patients who have been admitted and discharged from the hospital since March 2020.
Last week we recorded the lowest number of Covid patients that we have diagnosed in the emergency department since last June. We’re still seeing cases but it’s not unusual for a doc to not have any positive patients during their shift (we staff 7-9 docs a day so odds are, we have at least one doc managing a COVID patient). Cases were so sporadic last summer, we actually went 2 weeks in a row in the middle of June without diagnosing Covid in an ER patient. (We’re not there yet) The numbers started to tick up by mid-July when Delta was coming to the area. And while September was the peak of the Delta surge, fortunately enough people had been vaccinated, the weekly numbers were typically less than half of what we were seeing during the winter surge last December and January.
Our COVID isolation numbers in the ED have been pretty stable over the last 3 weeks. We’re better than a month ago but we continue to have a steady number of patients who require our COVID isolation protocol. Hospital wide, our inpatient census is up a touch from last week and our overall percent positive rate for the hospital is also up a bit. We are starting to see just a sprinkling of flu cases over the last month. It’s not too late to get your flu shot. I’m sure I’ll be talking more about flu in the coming weeks.
Vaccination rates are excellent in the area, and I love seeing so many pictures of the younger kids get vaccinated. However, as a country, there is still obviously room to go improving vaccination rates. We had a positive patient this week who had refused vaccination. The patient’s doctor sent him to the hospital for monoclonal antibody treatment. The patient also refused that and generally refused to believe that Covid was the cause of their illness. There is still a lot of misinformation out there and all of us have responsibility for helping to share our experiences and the truth.
While I would love to see a week without any positive cases, the handful of cases that we have gotten each of the last couple weeks is likely to stay with us for the time being. Overall, this is good news and really speaks to how the Covid pandemic is changing to a virus that is endemic.
Let’s review some basic definitions again. An epidemic is when a disease affects a community or region. Pandemic is disease across countries or continents (world-wide). Whereas, endemic is a disease found within a population or country. Malaria is endemic to parts of Africa. We’ll likely continue to see COVID cases around the world for some time much like measles, with COVID playing a recurring role in the US.
Reuters published an article this week about how the pandemic should transition to an endemic disease state in 2022. The World Health Organization is hoping to have 70% of the world’s population vaccinated by the end of 2022. If there are no major mutations that would render the vaccine ineffective, the US and other highly vaccinated countries should be among the first to be out of the pandemic. Cases and deaths have been declining since August all over the world though there are countries seeing a rise in cases (often correlated with low vaccine rates or little mask wearing). Most experts do predict a modest increase in cases this winter and expect it to cause more deaths than the flu. However, unless a highly virulent strain evolves, perhaps the worst is behind us.
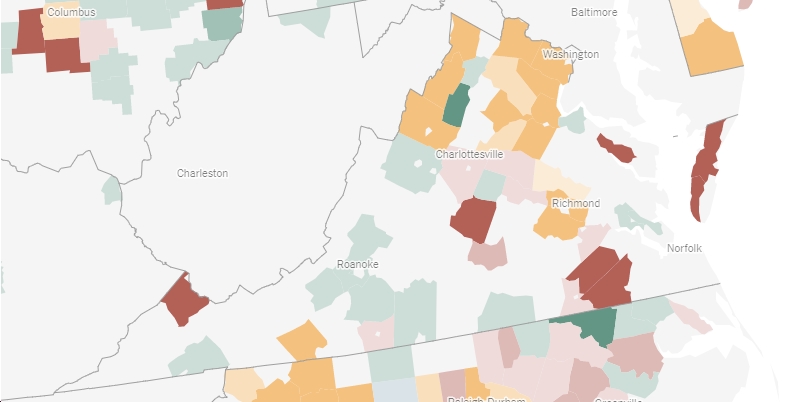
Unfortunately, this does not mean we return to pre-pandemic social interaction. Israel is about 2 months ahead of us from a vaccine perspective and they’re having an increase in hospitalizations and death. Europe is also seeing increases in cases (the Netherlands is looking at a partial lockdown) and the World Health Organization reported that Europe had 2 million cases last week, making it the most cases in a week since the pandemic began. Eastern Europe has lower vaccination rates, but case numbers have also increased in highly vaccinated parts of Western Europe. Closer to home, there’s some hotspots in the Mountain West and in the North, likely related to low vaccination rates, few mask mandates, and cooling temperatures with people moving inside. There was an outbreak after Halloween parties at a college in Vermont and hospitals in Detroit, Colorado, and New Mexico are having increases in patients. Two New Mexico hospitals are looking to delay elective procedures because they’re focusing on their sickest patients. While many people have tried to return to their pre-pandemic life, masks continue to help you be safe and boosters will also have a role to play. And while I’ve talked about medications expected down the road to prevent hospitalization, reducing the number of new cases is still critical.
Although many people have pandemic fatigue, it’s still important to remember to get tested when you’re symptomatic, quarantine if you’ve had a high-risk exposure or think you could have COVID, and let your contacts know if you’ve positive and exposed them.
Finding a rapid antigen test at your local drug store isn’t easy to begin with but it’s likely to get a bit tougher. The FDA is recalling up to 2 million Ellume rapid antigen tests because they produce “higher than acceptable false positive result.” Although, the FDA is only reporting 35 false positives as being reported.
There is some good news on the horizon. Pfizer is seeking FDA authorization to give a booster to those 18 and older. This is great news and I’ve been anticipating this for a couple of months. Even in my personal life, I’ve seen an increase in breakthrough cases among friends/contacts. We’ve seen plenty of data that vaccine efficacy is 40-60% by 6 months. Although the vaccine will keep you safer from hospitalization and death than being unvaccinated, the overall preventative efficacy decreases over time. Even having a mild case of COVID is disruptive to your life/home/job/school and puts others at risk. Now Pfizer has the data on 10,000 patients who received boosters and it looks like the efficacy rate gets back to 95% against symptomatic infection. In that study, there were 5 cases of symptomatic infections among the booster group compared to 109 among the placebo group. The FDA is set to review the data and make a recommendation that will then be carried to the CDC for final approval. CDC Director Rochelle Walensky approving this is not a given. There is some concern about the risk of vaccine associated myocarditis in 18-29 year old males. I’ve seen possible booster age cutoffs of 30 and 40 years and up discussed as younger vaccinated people generally have mild cases of COVID. However, several countries have been widely giving boosters over the last couple of months. Israel offers them to 12 and up and Canada approved boosters for 18+ this week. And this week, they were approved for 18 and up in both California and Colorado.
What we don’t know yet is how long the booster will last. We’re watching science play out in real time. We don’t have long term data, but the short-term data shows antibody levels 1-2 months out look good. The logic is that the booster will last 6 months and likely longer, just like other vaccines that require a series of shots (I showed my son’s vaccination records recently as a reminder to how many shots kids get) One difference between COVID and the flu is that the flu vaccine components change every year reflecting the different strains the vaccine is trying to protect against. While certainly COVID vaccines may evolve to protect against different strains, the current vaccine is doing well to protect against the existing mutations.
I got asked last week my take on the CMS guidelines requiring vaccination for healthcare workers by January 4th. Fortunately, as a doctor, it’s not hard for me to endorse getting vaccinated. I know many doctor’s offices, hospitals, and states that have already required it. I’ve also talked to physician friends who had staff quit rather than get vaccinated and that has made their work even more challenging. I heard this week that 500,000 healthcare workers have left the industry since the pandemic began, so there were already significant staffing shortages in all aspects of healthcare. I suspect many people are trying to balance individual rights, patient safety, and having enough workers to care for patients. Ten states (most rural) have filed lawsuits over the mandate based on individual and state rights with concerns about exacerbating workforce shortages. Workforce shortages is a real concern. I don’t envy the hospital executives who have been making these decisions over the past year. The VHC vaccination rate is really high despite a lack of mandates though not 100%. Of course, the CMS regulation will allow for religious and medical exemptions so I don’t think any hospital will get to 100%.
Science matters. Get vaccinated (or your booster). Wear a mask. We’re almost there.
Mike