Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
Yesterday was the anniversary of the first case of COVID diagnosed in America. Since then, we’ve had over 69 million confirmed cases and 860,000 deaths, with still more than 2500 people dying per day.
In the grand scheme of things, the Omicron variant is milder than Delta. However, there’s a great article in the Post from earlier this week that focused on an ER in Rhode Island where it’s very clear that the ER was being overrun by COVID patients. The rate of new cases in Rhode island was in excess of 400 per 100,000 people and the ER chair was extraordinarily honest about the chaos they were facing and the collapse of the “safety net” that the ER has always provided.
Although Omicron is still surging throughout much of the US, it does appear that around NoVa, we’re declining from our peak. In the ER, new case numbers have fallen 65% from our peak 4 weeks ago. Our overall percent positivity rate in the ER has been as high as 45% recently and is now about 22% (goal <5%). The number of symptomatic patients who were testing positive has fallen 75% and the positivity rate for testing symptomatic patients has declined from 66% to 33%. We are moving in the right direction.
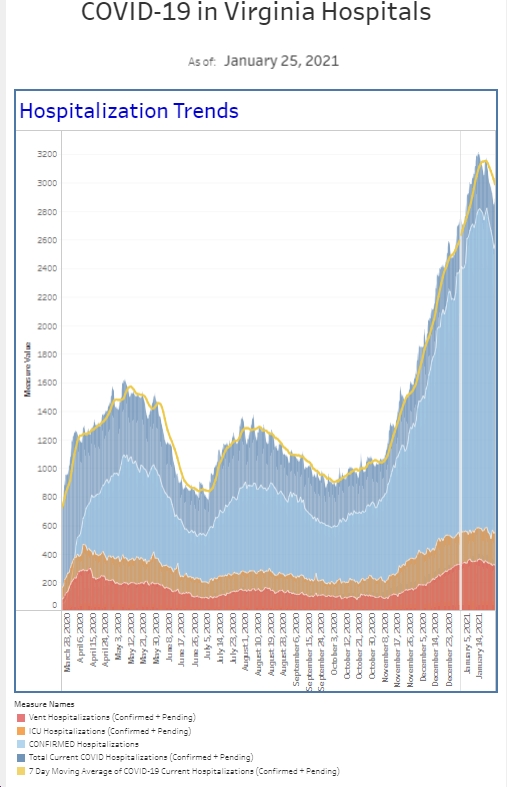
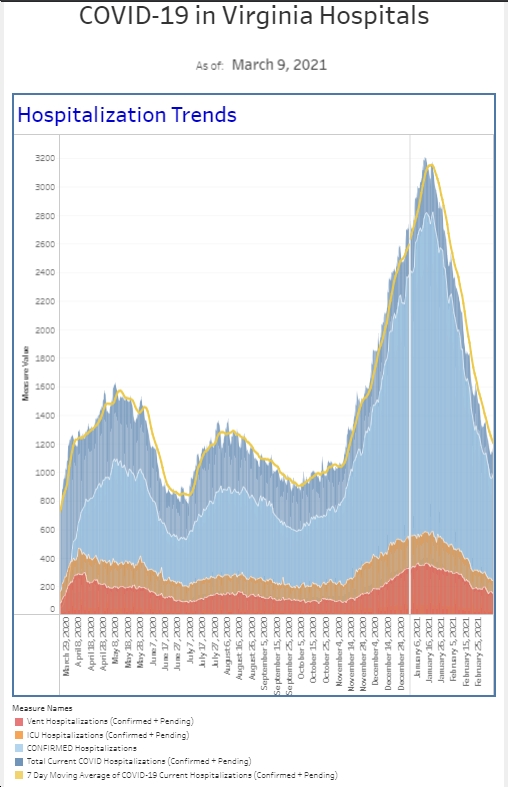
With that said, the numbers are still 3-5 fold higher than in the fall. We’re still seeing plenty of COVID and people are still dying with COVID, but as an emergency department, we’re able to take a breath and we appreciate the surge is coming to an end. Our inpatient census is also down 30% percent from the peak. However, it’s basically 80-90% of previous peaks, but it’s nice to see the downward trend. Just like hospitalizations and deaths lag 2-3 weeks behind case numbers, the hospitalist and ICU teams (doctors and nurses) are still really busy. Hopefully, their workload will return to a more normal number over the next few weeks.
In my mind there is a difference in how I act personally (going to restaurants or wearing a KN95 in public) between where we are now (post peak) and where we are when there are low levels of COVID circulating in the community. There are times where we can go back to a more normal pre-pandemic life. We’re not there yet. We still need to exercise caution in our daily activities.
There’s a very preliminary study out of Israel looking at the benefit of a 4th dose of vaccine. 274 healthcare workers received either Pfizer (154) or Moderna (120) as a 4th dose. Each group had an increase in their antibodies to COVID but it appears this increase is not sufficient to prevent omicron infection. Although the 4th dose did boost antibodies to a level higher than the 3rd dose, it still isn’t believed to be enough to consistently prevent against infection. While it’s a small study, the authors suggest the results do not justifying giving a 4th dose to the whole country,
So this brings us back to a basic question about the benefits of the vaccine. While the vaccine was clearly beneficial in preventing infection, the virus has mutated enough to feel like you’re wearing armor. However, vaccination clearly prevents severe disease and death when looking at vax vs unvax patients. We’ll likely see another version of the vaccine directed towards Omicron in the near future. And while this surge subsides, the big question is not if there will be another variant that causes a surge, but when. The virus will continue to mutate until there is worldwide immunity (from either vaccine or having the disease).
Hopefully everyone has ordered their 4 free antigen test kits from the government. We have used up a bunch of rapid tests at my house recently, after not really needing many over the last 6 months. The tests are a nice tool in helping us manage COVID but there’s a good study that looked at PCR tests versus antigen tests on healthcare workers who were tested daily. First, with Omicron, it seemed like saliva (back of throat) was more reliable than nasal swabs. Peak viral load was 1-2 days faster in saliva than nasal secretions. Second, the average time from positive PCR to positive antigen test was 3 days. All individuals had symptoms within 2 days of the first saliva PCR test. That means you were contagious before you had symptoms and most likely before your rapid antigen test was positive. Therefore, if you’re exposed, and asymptomatic, you should probably wait 5 days before you test with a rapid test. And if you test on day 3, you’re best testing again on at least day 5 and also day 6 or 7. Then if you’re negative and asymptomatic, you will most likely stay that way. If you’re positive at any time, then you’re positive and isolate. This is particularly true if you’re also symptomatic.
Although it seems there’s still people who don’t believe in the vaccine, the CDC released a really interesting study today in it’s MMWR comparing the incidence of COVID and COVID related death rates in 25 jurisdictions among unvaccinated and vaccinated individuals (+/- booster). Here’s a couple of key sentences from the paper. “During October–November, unvaccinated persons had 13.9 and 53.2 times the risks for infection and COVID-19–associated death, respectively, compared with fully vaccinated persons who received booster doses, and 4.0 and 12.7 times the risks compared with fully vaccinated persons without booster doses. When the Omicron variant emerged during December 2021, case {risk} decreased to 4.9 for fully vaccinated persons with booster doses and 2.8 for those without booster doses, relative to October–November 2021. The highest impact of booster doses against infection and death compared with full vaccination without booster doses was recorded among persons aged 50–64 and ≥65 years.” The vaccine was developed against the original virus. It does become less effective as the virus mutates but continues to offer protection. Although it’s unclear exactly where boosters are heading, study after study continue to show that vaccination saves lives.
In a separate paper released today as well, the authors looked at the impact of booster shots on reducing ER and urgent care visits as well as hospitalizations. “Vaccine effectiveness following a third dose and was highly effective during both the Delta- and Omicron-predominant periods at preventing COVID-19–associated ED and UC encounters (94% and 82%, respectively) and preventing COVID-19–associated hospitalizations (94% and 90%, respectively). It’s not too late to get your booster.
Two years in and everyone is exhausted. Personally, throughout the entire pandemic, I’ve kept focused on the end of each surge either through predictive models or through evaluation of my own data. Marathons are really tough races but you know their end point. Early on in the pandemic, we felt like the finish line kept being moved. And while the ultimate end to the pandemic remains uncertain, the surges are more predictable.
The Coronavirus is not done with us yet.
Science matters. Practice physical distancing. Get vaccinated (or your booster). Wear a mask.
Mike