Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
The Omicron surge really reset the bar for how crowded the ER could get and how many cases of COVID a week we would see. A month ago, we were setting records for daily and weekly volume and total number of COVID patients diagnosed. The view this week looks a lot better. But it’s relative to where we were a month ago. Our total number of weekly COVID patients is still higher than the beginning of the surge and higher than we saw during the Delta surge in late summer. The total number of COVID patients we’re diagnosing in a week now is about 3 times higher than our Delta peak and is about the peak of where we were during last winter’s surge. While the numbers are better than a month ago, I suspect we still have 4-6 weeks until we start to get back to low tide. Our overall percent positive has dropped from about 40% to 18% which is just a touch below last winter’s surge but twice as high as the Delta surge. The public health target for percent positivity is <5% and ideally at some point, we’ll get to <1% (at the local/state level), and then we’ll see a much more return to normal in our daily life.
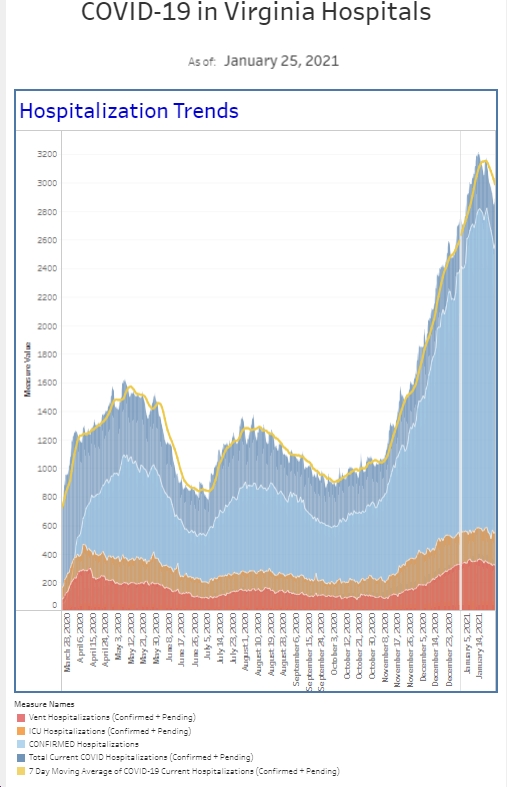
The number of patients who present to the ER and require COVID isolation continues to trend down, About a month ago, half of our patients required this procedure. Now, it’s about 20%. The number is similar to the first couple weeks of the surge in mid-December, higher than the Delta surge, and a tad below the surge last winter. The number of COVID patients hospitalized is also down about 20% from last week, yet still double the number we had just prior to Christmas. Our hospitalist team is still so busy they’re requiring staffing with an extra physician.
I’m on vacation this week, which pretty much means working from home. I was supposed to be at a conference in Florida, but it was cancelled due to COVID. I did take my son to Orlando last weekend for a soccer tournament. It was my first time traveling in 2 years. My wife has been traveling for work throughout much of the pandemic and has been fine. I wasn’t so much against travel as I just didn’t have anywhere to go. We wore N95s on the plane, much to my son’s displeasure. Despite it being 45-50 degrees in Orlando, we were generally outside as well. I have to admit, it was really good to travel again, and we hope to do more of it, preferably with better weather and less soccer.
A good part of this week has been dedicated to continuing medical education. I’m knocking out some of the requirements for maintaining my board certification. Included this week were completing online tests on emergency medicine topics that had nothing to do with COVID. Whenever I do board certification stuff, I’m reminded of all the great cases emergency physician’s handle. It’s a wide breadth of patients we manage though certainly over the last 2 years, it’s been heavily influenced by COVID. It was a bit surreal to do that much CME and not have anything related to COVID.
I get a lot of daily emails with COVID information. What was so interesting about one of the emails was the top story was evidence that Omicron causes less severe disease than previous variants. From the CDC, “Despite Omicron seeing the highest reported numbers of COVID-19 cases and hospitalizations during the pandemic, disease severity indicators, including length of stay, ICU admission, and death, were lower than during previous pandemic peaks.” Don’t get me wrong, this is great news and consistent with what we’re seeing in the hospital. However, the next story reported “seven-day average for new COVID-19 deaths in the US reached 2,191 per day as of Monday, marking the highest level since early 2021 and up nearly 1,000 deaths from two months ago.” And this is the giant disconnect we see as healthcare workers who are exhausted and still battling a hospital full of COVID patients while portions of society are saying the pandemic is over. People hear that Omicron is mild and think they can go about their normal lives while hospitals are overwhelmed by the sheer volume of patients requiring care. Yes, the percentage of people who require hospitalization is less but the total volume of patients requiring care is higher.
When hospitals are full, as they are now around the country, admitted patients often have to wait in the ER for an open bed upstairs in the hospital. We refer to this as “boarding.” Every ER has some boarding. Some hospitals board more than others. We’ve been talking about it and studying it or 20 years. Published recently, in a pre-pandemic study looking at 5 million cases from the UK between 2016-2018, the authors linked prolonged time in the ER to an increase in death rates. They evaluated 26 million patients who came to the ER over the 2 year study period. Almost 7.5 million were admitted. 434,000 people died by day 30. The authors then went and looked at arrival time to ER to leaving the ER to go the inpatient unit. Mortality increased 8% for patients who spent more than 6-8 hours in the ER from time of arrival. This equates to 1 extra death for every 82 patients admitted whose time to inpatient transfer was beyond 6-8 hours. My understanding of ER flow in the UK is that it’s bit different than the US, however other studies have reported poor outcomes associated with ER boarding. And during these surges, most hospitals have experienced record number of boarding hours. Besides increasing hospital mortality risk, there is also a trickle down effect of how boarders cause delays for ambulance patients getting offloaded, which then keeps ambulances from responding to new 911 calls. You can imagine potential consequences. Recently, my own county in Maryland tweeted that there were no ambulances available to get patients and that Fire Engines would be responding and transferring patients.
There was a large study on physician burnout that came out this week. There’s always a percentage of physicians in all specialties that are “burned out.” I used to participate in a burnout study every year and stopped doing them long ago because my results would say I was burned out when I felt really good about the work I was doing. With that said, emergency medicine had the highest rate of burnout among physician specialties this year. Our rate was up 50% compared to last year. In a related study out of Mayo Clinic proceedings, 1 in 5 physicians expect to leave their practice in the next 2 years due to burnout, workload, or stress associated with COVID. Nurses were 2 in 5. And 1 in 3 docs, nurses, and advanced practice providers (PAs and NPs) intend to reduce their hours in the next 12 months. This obviously has huge workforce implications when it comes to staffing hospitals to provide care to patients down the road.
Let’s really switch gears and talk fertility as concerns regarding fertility are often raised by vaccine hesitant people. First, the CDC released results earlier this month on the safety of the vaccine during pregnancy. We know that pregnant women who get COVID are at increased risk for severe illness and bad outcomes. Now, in a review looking at 40,000 pregnant women, researchers showed that vaccination during pregnancy was not associated with preterm birth or small-for-gestation age births. In other words, getting vaccinated during pregnancy is safe. There was a second study looking at the impact on vaccine on patients undergoing IVF compared to unvaccinated patients. There were similar ferritization rates to unvaccinated (80.7 to 78.7%) and also vaccination was not tied to other early pregnancy outcomes. These studies add to the literature that vaccinating does not negatively impact fertility. The CDC also recommends getting vaccinated if you think you might become pregnant in the future.
While I’m glad we’re seeing improvements in the numbers, we are in a waiting game for the next variant to arrive. There is a variant worth knowing about right now. It’s Omicron’s cousin, the BA.2 variant. The original Omicron is now referred to as BA.1. The new version is already on 4 continents, with cases found in several states as well (including California and Texas). The primary difference with Omicron is seen in the spike protein. Omicron was only the 5th variant of concern as deemed by the WHO. BA.2 hasn’t reached that level yet. Denmark is having a higher rate (about 45% of cases) of BA.2 and fortunately the severity of it appears similar to the original Omicron. There was concern that natural immunity caused by Delta might not hold up against Omicron, but it is believed that immunity from BA.1 should work against BA.2. The current belief is that the vaccines will perform similarly, as will the new oral medications by Pfizer and Merck.
Both Pfizer and Moderna have started clinical trials to evaluate a vaccine that targets Omicron. The potential for this was brought up in mid-December and expected to take several months to get data and potentially to market. If you have not gotten your booster yet (and about 50% of eligible Americans haven’t), now is the time to get it. However, for those of us who received boosters, a new recipe has the potential to be what we get as a 4th dose this spring. The Pfizer CEO is optimistic that a new vaccine will be ready for March and will target multiple variants.
Published in JAMA this week is a large study looking at the association between myocarditis and vaccination. Over 190 million people received over 354 million doses of vaccine. There were about 2000 reports of myocarditis with a median age of 21 and a median to symptom onset of 2 days. Males made up 82% of the cases with rates higher after the second dose. Rates of myocarditis were: 12-15 year old (yo) 70.7 per million doses, 16-17 yo 105.9/million doses, and 18-24 yo 56.3/million doses. About 96% of these patients were hospitalized, 87% had resolution of symptoms by discharge, and 87% were treated with NSAIDs (like Motrin). The risk of myocarditis from COVID is about 150 cases per 100,000 patients (note the difference in case number per hundred thousand versus million) and this rate is 16 times higher than the general population risk of about 9 cases per hundred thousand patients without COVID. While there is a very small risk of getting myocarditis from the vaccine, particularly if you’re a teenage male, the benefit appears to far outweigh the risk.
The other important CDC study published this week had to do with the impact of a booster on preventing hospitalization for both healthy and immunocompromised patients. Data was obtained during the Delta surge and into early December but does not include the Omicron surge. Vaccine effectiveness against hospitalization was 82% for people who got 2 doses (compared to unvaccinated) but goes to 97% for boosted patients. For the immunocompromised, the number increases from 69% to 88%. Boosters will help keep you out of the hospital.
The Coronavirus is not done with us yet.
Science matters. Practice physical distancing. Get vaccinated (or your booster). Wear a mask.
Mike