Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
We continue to see improvements in the number of COVID patients that we are diagnosing. In my last shift, I actually did not diagnose any patients with Covid. That is pretty amazing. However, I saw several patients with persistent shortness of breath 2-3 weeks after having COVID and despite a fair amount of testing, I wasn’t able to determine a cause. I haven’t written much about long COVID because we don’t typically see it in the ER, but I do wonder if we’ll start to see more Omicron patients who present with persistent respiratory symptoms.
We have seen the number of patients who present with symptoms that we diagnose come down by about 90% over the last 6 weeks. Our 6-week percent positivity running average for this category of patients is 54%. A month ago, it hit its high point of 64% but is currently 21%. We were diagnosing more than 200 patients a week who presented with symptoms a month ago and now, over the last couple of weeks, we’re in the range of 10-20 patients/week. Among our general screening patients (who should not have symptoms such as cough, shortness of breath, fever etc.) the percent positivity rate has dropped from a recent high of 31% to about 11%. We’re actually seeing more patients in this category test positive each week than among our symptomatic patients. But to be fair, we are testing about 8 times more patients for general screening than symptomatic patients. When we put all of this together, the 6-week percent positivity average for all tests done in the emergency department is 32% and our testing positivity rate last week was about 12%. The total numbers of positive cases have declined from about 400 a week to 60 this past week. The overall percent positivity rate is still higher than most of 2020, but is consistent with the end of last winter’s surge. We are also still diagnosing more people with Covid each week then we did between February and December 2020.
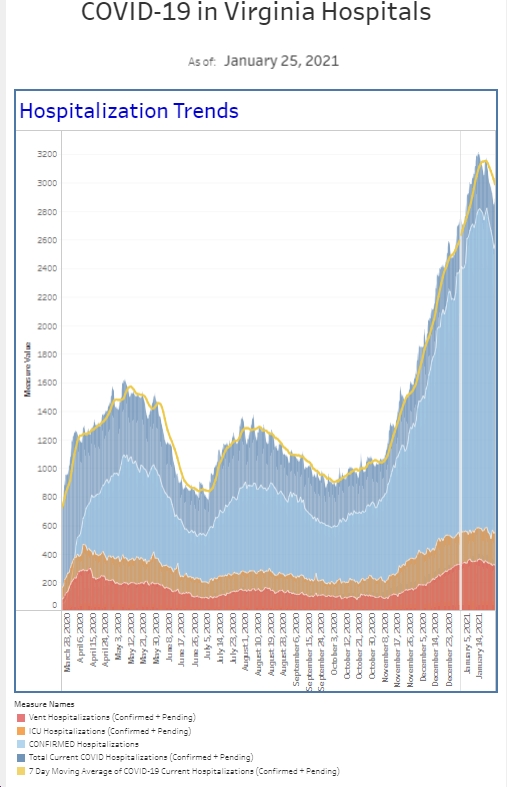
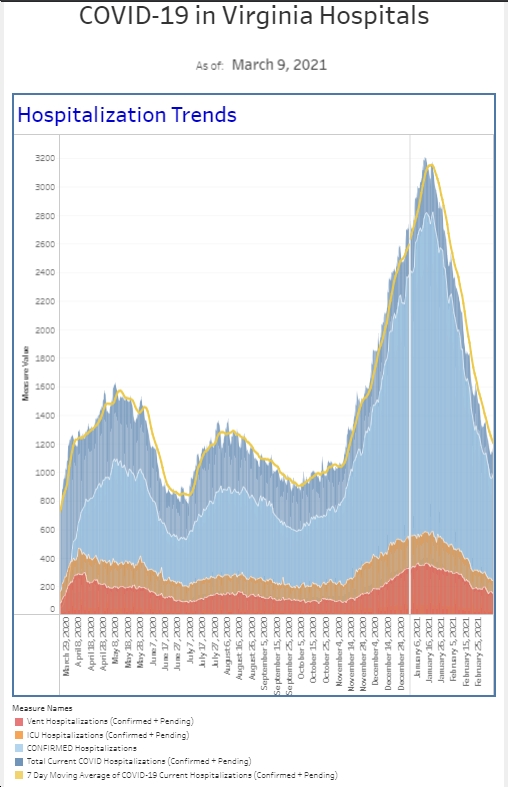
The number of hospitalized patients is also down about 60% from our peak a month ago. And we continue to see improvements in the number of patients who require Covid isolation in the emergency department.
Although numbers are looking better around the hospital, our Stealth variant, the BA.2, subvariant of omicron, appears to be more transmissible than the BA.1. In a Danish study of approximately 8500 households between December and January, it appears that people “infected with a BA.2 subvariant were roughly 33% more likely to infect others, compared to those infected with BA.1.” The BA.2 variant certainly remains a concern as do other variants that we may not even be aware of.
About 25% of the population remains unvaccinated. Many of these people have thought they had COVID but were never tested. Let’s be honest, many of us, particularly in healthcare, assumed we had it at some point. Now a study published in JAMA looked for evidence of previous infection based on antibody testing in unvaccinated patients. 1580 unvaccinated patients were recruited from social media and answered a questionnaire online. Patients were grouped into 3 categories: confirmed COVID infection, believe they had COVID but were never tested, and did not believe they ever had COVID and were never tested. Patients then underwent antibody testing. Of COVID confirmed patients, 99% had antibodies. Among the patients who thought they had COVID but didn’t have confirmation, only 55% actually had antibodies. And for those who didn’t think they ever had COVID, 11% actually had antibodies. If you previously thought you had COVID but were never tested, it’s potentially 45% likely that you did not have it.
The data for the benefit of vaccination continues to come in. The CDC published a paper this week in MMWR, looking at the COVID incidence and hospitalization rates in Los Angeles County during the early winter when omicron was the predominant variant. Unvaccinated people were 23 times more likely to require hospitalization compared to vaccinated patients with a booster and 5.3 more times likely to require hospitalization compared to those who are fully vaccinated but did not have their booster. The incidence of testing positive for unvaccinated people was 2 times more likely the most fully vaccinated without a booster and 3.6 times more likely than those vaccinated with a booster. Getting vaccinated clearly protects you from getting hospitalized if you get COVID and adding a booster is even more protection. The vaccine also helps keep you alive if you get COVID. Unvaccinated people are 14 times more likely to die than vaccinated people (2 shots) and 97 times more likely to die than those who are vaccinated and boosted according to CDC Director Dr Walensky during a briefing this week.
Over the last 2 years, I have had many discussions with friends with unvaccinated young kids about their stress with kids going to school as well as keeping them safe. I am stressed for them and also appreciative that my kids are older and vaccinated. I have 3 very good friends with young kids not eligible for vaccination who are all wresting with COVID positive kids this week, and Covid going through their households because their kids got exposed and ultimately sick through daycare. One of them will ultimately have her kids out of daycare for a month due to exposure and quarantine rules. Of course, this has the downstream impact of keeping her and/or her husband out of the office and home from work as well.
I am so thrilled that US regulators encouraged Pfizer to apply for emergency use authorization for the 2 dose vaccine for children 6 months to 5 years old and Pfizer did so this past Tuesday. The FDA vaccine committee will meet on February 15th to discuss an EUA request, taking us one step closer to approval for this critical age group. This will allow kids to get started while the data still comes in on the benefits of a third dose. Pfizer considered submitting this data last year. The data shows that the vaccine is safe and effective, but Pfizer did not think the 2 days shot was as effective as it should be in this age group. That is why they wanted the study the impact after the third dose. Data from the third dose should be in in late March. By granting EUA in the near future, younger kids will be able to start the vaccination process.
We all remember washing the groceries and everything we touched really well at the beginning of the pandemic. I was never one to wipe down my workstation prior to starting his shift but I definitely did at the beginning of Covid. As the numbers improved last summer I actually stopped being so diligent with cleaning my workstation. Even as the winter surge came on, I was not as worried that I could get Covid from my keyboard or phone. Now there is research out of Duke supporting that much of that cleaning was not necessary. Samples were taken from multiple surfaces in the rooms of 20 Covid patients over their first 2 weeks of hospitalization. Of 347 samples, only 19 were positive for Covid by PCR. 16 of these 19 samples were obtained within the first 3 days of the patient’s hospitalization. Of the 19+ samples, only 1 have the potential to be infectious, and this was from the bed rails of a symptomatic patient with diarrhea and fever. One thing to keep in mind is that while hospital rooms do get cleaned, they are not sterilized while patients are in the room. The authors conclude that small amounts of viral particles detected on surfaces are not a high risk mode of transmission. This study is further evidence that COVID is an airborne disease and that prevention should continue to focus on masking, physically distancing, and ventilation.
The Coronavirus is not done with us yet.
Science matters. Practice physical distancing. Get vaccinated (or your booster). Wear a mask.
Mike