Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
The BA.5 subvariant of Omicron now makes up 78% of new COVID cases in the US. Recall that this variant is highly transmissible and is resulting in the current uptick in cases we’re seeing. Lots of people think they’re having allergies, only to ultimately find out they have COVID. I’ve also seen a lot of patients who initially had negative rapid tests only to subsequently go on to test positive by rapid test or PCR (one rapid test doesn’t mean you don’t have COVID—if you’re still symptomatic a day or two later, test again). In a recent survey of >17000 UK patients, the most common symptom was sore throat (58%). “49% had a headache, 40% had a blocked nose, 40% had a cough without phlegm, and 40% had a runny nose.” These symptoms sure can be confused with allergies. I’ve seen a lot of patients who don’t typically get headaches present to the ER with pretty bad headaches. You know what’s not on the list? Loss of taste and smell, now only 13%. Although only 27% of people reported fatigue, when I’m talking to patients that have COVID related fatigue, it’s pretty severe.
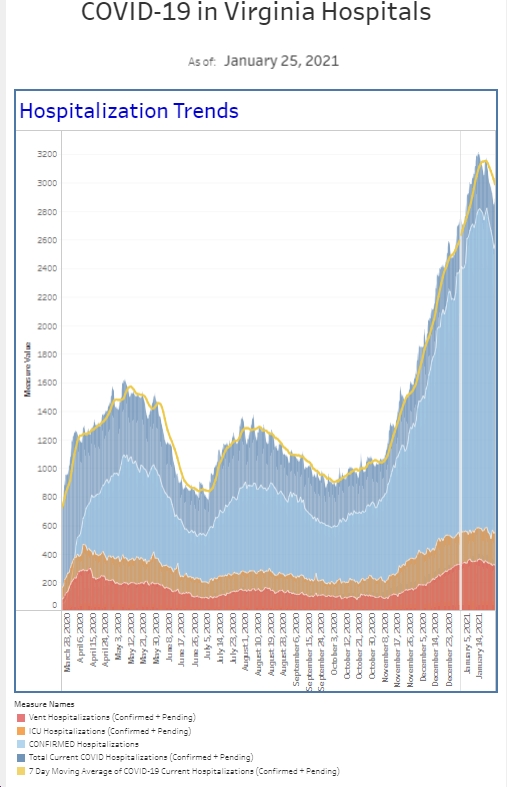
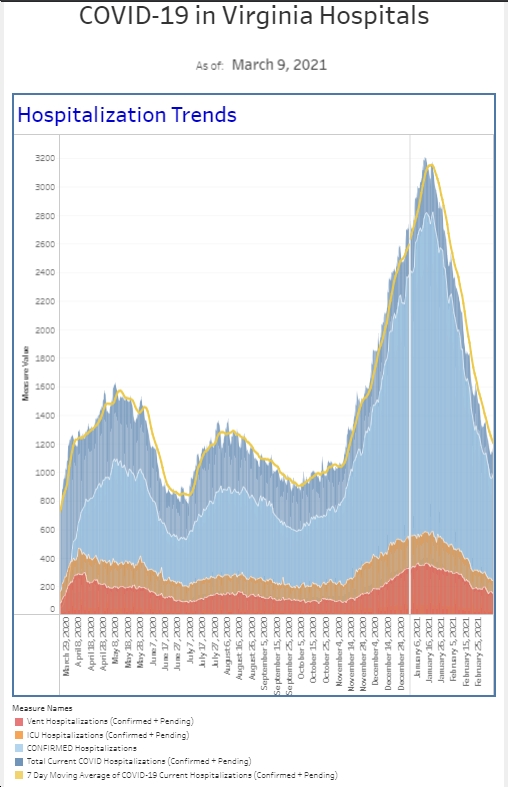
For the third week in a row, we’re diagnosing more patients with COVID than we did the week before. For the 8 weeks before that, our numbers were fairly constant, bumping up or down a handful of patients each week, but generally in the same ballpark. Last week had 50% more positives than that 8 week average. Among our symptomatic patient population, the number of cases and the percent positivity rate are the highest they’ve been since late January. The total number of patients we’re diagnosing is similar to the first waves we saw in 2020, though is still far below the huge numbers we saw with the Omicron surge last January. The good news is that while the number of patients requiring hospitalization is creeping up, the numbers are not as high as they’ve been with other surges with only the occasional patient requiring the ICU.
Keeping patients out of the ICU can definitely be attributed to vaccinations. Although the mRNA vaccines are not as effective against these variants as they were a year ago against the original strain in preventing infection, they do remain effective at preventing significant illness and death. There was a nice study published by the CDC in MMWR this week looking at potential benefits of first and second boosters in preventing moderate to severe disease. The authors looked at real world data between December 2021 and June 2022, during the Omicron surge and the initial subvariants in all age groups. Although vaccine effectiveness (preventing infection) declines over time, a booster increases the effectiveness. More importantly, vaccine boosters significantly reduce your chances of needing hospitalization or dying. The authors found that a booster (3rd shot) reduces the risk of moderate to severe COVID in all eligible persons and that a second booster (4th shot), four months after the first booster provides extra benefit to those 50 and older. Yet, large numbers of eligible patients have not received a booster and the majority of people 50+ have not received their second booster.
In a separate analysis of CDC mortality data, physician scientist Dr Eric Topol wrote that your risk of dying from COVID is 29 times less likely if you’re vaccinated with 2 boosters compared to the unvaccinated. And even if you have one booster, you’re 4 times less likely to die of COVID if you get your second booster.
I had some déjà vu this week during a Monkeypox testing strategy call. Just like in the beginning of COVID, we had to work with the health department to get patients tested for COVID. And pretty much tests would only be run on patients after we tested for other things that led to similar patient presentations. For Monkeypox, this would include testing for varicella (the virus that causes chicken pox and shingles) and herpes. These are not tests that result rapidly in the ER which means patients may be swabbed for Monkeypox but the state would only run it after the other tests come back negative. This can send mixed messages to patients about the etiology of their illness, which can lead to noncompliance on the isolation side. COVID was similar in the spring of 2020. With Washington, DC being among the top cities with diagnosed cases of Monkeypox, I hope we can streamline testing to provide more rapid results to patients. I personally haven’t seen any patients yet that required testing for Monkeypox. On the other hand, I worked in the ER last night and didn’t see any COVID patients either and I know COVID hasn’t disappeared.
Ivana Trump died from a fall. I missed this in the news cycle initially and it seems that many are surprised you can die of a fall. Falls, particularly in elderly and/or mixed with alcohol are incredibly common. Falls in the elderly are among the top reasons for our trauma activations. I think I had 3 patients last night who came in because of falls. While many people obviously fall without significant injury, we also see the other side of the spectrum where people have devastating bleeds into their brains, break their necks, or have other internal injuries. Wearing shoes when walking, holding on to bannisters, not having your hands occupied by carrying items, and not walking stairs while intoxicated reduce your risk of falling, particularly in the elderly. We also see patients who fall who may not have life threatening injuries, but they can’t get up and call for help. It’s not unusual for patients to lay on the ground for a day or two before someone finds them. By then, patients can have life threatening issues from muscle breakdown and dehydration leading to kidney injury. We may laugh at the memory of the “I’ve fallen and I can’t get up commercials,” but those devices can be literal life savers. Your apple watch also has a “fall” alert system that can notify an emergency contact. (While I’m at it, we also see a lot of patients fall off electric scooters. Please don’t drink alcohol and get on them and always wear your helmet when you’re on an electric scooter)
Coronavirus is not done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike