Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
Friday Night Update from the ER in Arlington, VA
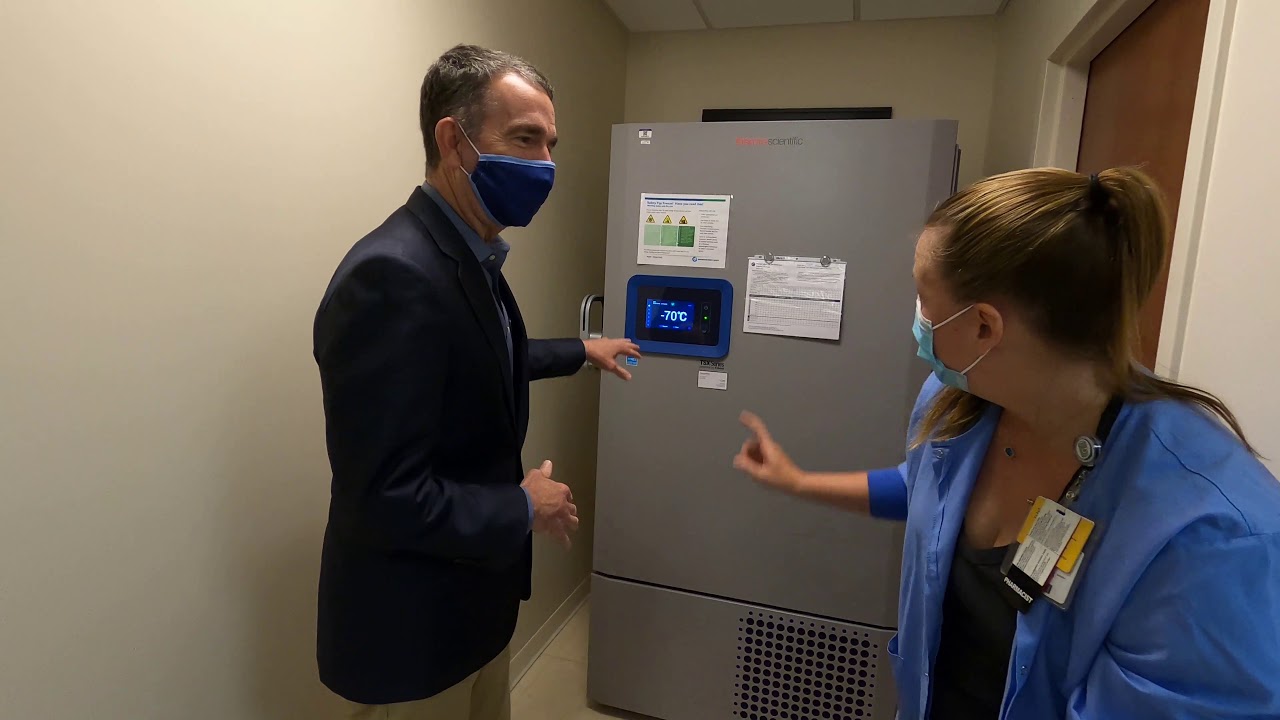
Both my daughter and I got our booster shots this week. We also both got our flu shots. She’s home for fall break and got hers at our local pharmacy and elected to get both shots in the same arm. All of her shots have been Pfizer and she got Pfizer this time since that’s what the pharmacy always seems to have. I got mine at the hospital before my Tuesday evening shift. All of my previous shots have also been Pfizer though this time I went with Moderna just to mix it up. I got 1 shot in each arm.
Besides some arm pain, I have never really had an issue feeling sick after the vaccine. I got my shot Tuesday around 11 AM, got home from work somewhere around midnight, and went to bed around 1 AM. Fatigue and sleep deprivation definitely goes hand-in-hand for shift workers. Throw on bio rhythms, parenting and making sure my son is up for school, and administrative responsibilities that are more of a daytime job than an evening job, and being tired is definitely something I am used to. I was really tired on Wednesday. I do not know how much of it was routine sleep deprivation versus the vaccine, but it did feel like my coffee did not have his usual affect to get me up and moving that day. My daughter has had some issues after previous shots but this time besides some arm pain and redness, she did really well.
The experts are predicting a heavy flu season. Projections are generally based on the flu season in the southern hemisphere during the summer. On top of that, public health experts are concerned about relaxed COVID-19 restrictions and returning to socializing without masks and people feeling more comfortable in large crowds. We have only had a small percentage of the normal flu cases that we would typically see during the winter over the last few years. The CDC is already reporting higher than normal expected cases of flu for this time of year, particularly in the Southeast and Southcentral US. Reported earlier this morning, a San Diego high school is reporting over 1000 absences on Wednesday out of 2600 students. While COVID testing has generally been negative, there have been a number of flu positive students, suggesting that this is potentially an early outbreak due to influenza.
Now is definitely the time to be getting your flu and COVID vaccines. And fortunately for the school-aged kids, the FDA has improved COVID boosters for all kids over the age of 5.
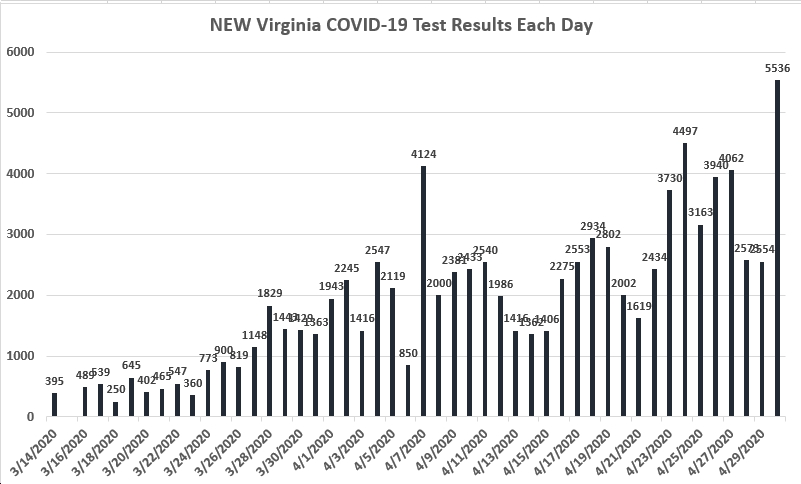
Now let’s take a look at the COVID volume in the emergency department. I saw a handful of COVID patients this week. A couple of them told me they did not think they had COVID because they had a negative rapid test earlier that day. We have definitely learned over the last several months, particularly with this variant, that one negative home rapid test does not rule out COVID. While it is great and accurate if it is positive, if you are symptomatic and the test is negative, you should consider getting a PCR test, or at least wear a mask and then retest in a couple of days. We started to see a decline in the number of patients we are diagnosing with COVID each week around the first or second week of September. Since mid-September, our weekly number of positive cases has been very stable. It’s certainly possible that this could be our new baseline norm until the next surge. Over the last 4 weeks, our percent positive rate has generally been about 6.6% and pretty stable as well. The number of patients currently hospitalized with COVID is down about 10% compared to last week. I admitted somebody last evening with COVID though I suspect they will not be in the hospital very long.
Now that COVID has been around for 2+ years, we’re starting to learn more and more about long-Covid. Published in Nature Communications, a study “based on the experiences of nearly 100,000 participants” in Scotland “found that between six and 18 months after infection, 1 in 20 people had not recovered and 42 percent reported feeling only somewhat better.” However, the study also found that “people with asymptomatic infections are unlikely to suffer long-term effects, and vaccination appears to offer some protection from long COVID.” We’ll see a lot more on long-Covid in the coming months I bet.
Ebola is back on my radar this week after an outbreak in Uganda. The CDC and Department of Homeland Security are routing travelers from Uganda into 5 airports so they can undergo a health screening, prior to entering the US. Dulles International is one of those airports, as is JFK, Chicago, Atlanta, and Newark. Our personal protective equipment (PPE) for COVID is nothing compared to what’s involved for caring for a potential Ebola patient, which literally involves shutting down about a quarter of our ER to help ensure staff safety.
This week we celebrated our nurses as part of Emergency Nurses Week. It takes a special kind of person to not only be a nurse but to also work in the emergency department. It takes an extra special person to work on the front lines of a pandemic. 2-1/2 years after the onset of the pandemic, there are still a lot of challenges that we face in the ER and in healthcare. We have a fantastic team here and I cannot thank our nursing staff enough for all that they do.
Coronavirus is not quite done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike