Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
Friday Night Update from the ER in Arlington, VA
By now, all of you have watched the video or at least heard about the Buffalo Bills football player Damar Hamlin who collapsed after a tackle on Monday Night Football. I am so thrilled with the recovery he is making.
I am not personally involved in the case and don’t know anything that hasn’t been reported in the news, but I will provide some background info on how ER docs think about that kind of injury as well as on one of the likely reasons that he may have collapsed.
Like many, I’ve had a lot of conversations with friends and colleagues about what happened (or what we think happened) and ER doc social media feeds were also filled with online discussions. From a big picture point of view, when a player collapses like that, we think about injuries to the brain, the spine, and the heart. These can cause a sudden loss of consciousness, suspend your ability to breath, and cause your heart to stop. For any unresponsive patient, the assessment of the patient is pretty much the same. Are they arousable, are they breathing, do they have a pulse, and of course, with the sports injury, consideration of protecting the spine.
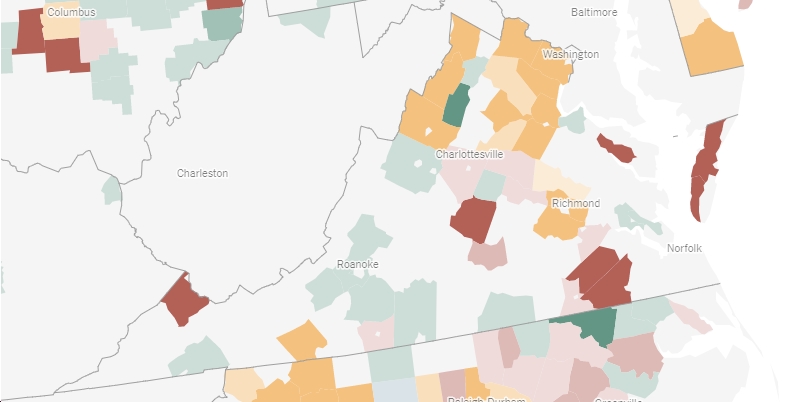
It is hypothesized that the player suffered from commotio cordis. This is an extremely rare injury that occurs when heart sustains blunt trauma during a critical portion of the heart electrical activity. I’ve attached a graphic. The timing of the trauma has about a 20-40 millisecond opportunity for an arrythmia during only a small portion of the electrical activity causing the heartbeat (see attached graphic). There is plenty of literature on commotio cordis and the original name goes back to the early 20th century (long before the COVID vaccine can be blamed). It’s estimated that 20-30 people die a year from it. Survival is estimated at 25% if resuscitation is begun within 3 minutes and only 3% if resuscitation is delayed beyond 3 minutes.
Most commonly, it’s seen in teenagers playing baseball, hockey, and lacrosse (particularly mens) though has occurred in other sports (I just read an article from 2009 looking at sudden death in lacrosse (1.46 deaths per 100,000 person years), which was similar to other sports though commotio cordis occurred more frequently in lacrosse with the exception of hockey—0.63 deaths per 100,000 person years). I’ve certainly read about cases of commotio cordis, though I’ve never seen a patient who had it happen to them, and I don’t believe I’ve worked in an ER that took care of a patient that suffered from it. There has been improvements to protective gear, particularly for lacrosse goalies, over the last decade.
Other athletes have suffered from cardiac arrest during games. You may recall that Denmark’s Christian Eriksen, a soccer player, had a cardiac arrest in June 2021. I followed that story closely. The likelihood of surviving a cardiac arrest is low, but I was definitely surprised when he was cleared to play again this year. Eriksen’s cardiac arrest was not a traumatic injury, so was different than commotio cordis. Both players did have a potentially fatal arrhythmia, requiring CPR and defibrillation. When you hear about athletes being saved, it’s because the site has an AED (at least) nearby which can shock the heart back into normal rhythm.
As people think about what we can do in our regular life to help save lives, learning CPR and making sure the gym or field you take your kids to has an AED can have a huge impact.
Now, let’s talk about the independent medical provider the news kept referring to. Each NFL team has an extensive list of healthcare personnel, including sports medicine physicians, orthopedists, chiropractors, and trainers, to name a few. Each NFL stadium also has the independent neuro consultant (for assessing concussions and return to play), as well as having an airway management doctor (which is usually an ER doc). When I worked for MedStar in Baltimore, I was one of the airway docs for the Baltimore Ravens. I did the role from 2006-2011, splitting the games with 1-2 other docs depending on the season. Between 8 home games, 2 pre-season games, not enough playoff games, and a couple of other sports (Navy football, NCAA lax championship, and European soccer), I spent plenty of time on the sidelines. I have several friends who have done or do the airway doc or neuro consultant role for NFL teams as well. Although, I’ve been off the sidelines for more than a decade, and the role has gotten more formalized, the nuts and bolts of it are still the same. The airway doc exists to take care of any player with a critical injury on either team. It’s a neutral role, although you’ll be able to identify the doc because they wear a red hat and are usually located around the 35 yard line, near the ball.
My understanding of the role is that is was created after a Minnesota Vikings player (Korey Stinger) died of heatstroke in 2001. He was off the field and it was after practice. For that reason, when I was an airway doc, we stuck around in the locker room until all the players from both teams had cleared out.
The airway doc has experienced paramedics working with them. I had basically the same pair of paramedics for the whole 5 years I did the job. We had a good routine and knew what our role might be. We got to the stadium 2+ hours early, went through our meds and equipment, and would try to meet with the other team’s medical staff. Since our job was really focused on airway and cervical spine management, we did drills in the pre-season with the training staff to work through the scenario of how it would work if a player collapsed, getting their face mask and shoulder pads removed, getting the patient secured on a backboard and into the ambulance, etc…One of the things we always had hoped was that if we ever had to intubate a patient, we’d be able to get them off the field, away from the fans and TV cameras. We thought we’d try to intubate them in the tunnel. But best practice is for the medical team to work the cardiac arrest right where it happens and that’s what we saw on MNF. It sounds like CPR and defibrillation were done on the field, then once a pulse was obtained, he was loaded and intubation took place in the ambulance off the field and away from the TV cameras. High quality CPR and rapid defibrillation give patients the best chance of survival. I did do some medical care on the sidelines and fortunately, for me, like almost every ER doc who has been on an NFL sideline, I never had to perform a lifesaving procedure on a patient. We are ideally there as an insurance policy and bring a very specialized skill set when there is a critical injury.
Back then, before the game, we would try to meet with the visiting team’s medical staff to introduce ourselves and talk through the equipment and carts available. Everyone is probably familiar with the cart that carries the player in the back while the doctor is next to them. That’s the team doc and not the airway doc. The airway doc and medics would be in the ambulance. Formal meetings with the medical staffs, airway doc and medics, and referees now take place prior to the game.
Watching someone undergo CPR is very disturbing. I’m glad the NFL postponed/cancelled the game. And for as much as I really enjoyed my sideline seat, despite managing a lot of cardiac arrests in the ER, I’m very glad I was never in the position of managing a player in cardiac arrest or in critical condition on the field.
A year ago, the ER had its busiest two weeks of the year. We had three days in a row of 250+ patients a day (pre-covid baseline 180). Omicron was surging and you couldn’t find rapid COVID tests at the pharmacy. We’re in a much better place but we did see a bump in COVID after the holidays as predicted. Our numbers started to rise around the 27th and we’re seeing the hospitalized patient counts also increase. We’re probably about half way to our max number of inpatients from last year but 2.5-3 times more than we had 4-6 weeks ago. I’ve admitted several patients with COVID over the past week.
Going back over the last almost three years, we’ve really had 4 big COVID surges with two smaller surges. The big ones were the initial couple of months, January 2020, January 21 and now (see the winter trend.) December 2020/January 2021 definitely changed our perspective of what a surge was because the number of positives we had and the percent positive rate were just so much higher than anything we had experienced previously. Last year, we got up to about 400 positive tests a week in the ER and an overall positivity rate of 40%. Our other surges were about 90 positives a week and a 20% positivity rate. Now, we’re seeing our highest numbers since the tail end of last winter’s surge with 100+ cases a week and a 20% positivity rate. Keep in mind, this data only applies to patients we test in the ER. There are lots of people testing positive with rapid tests and/or getting seen by their PCP or at Urgent Cares. For a full picture of what’s going on in Arlington, go to the county’s COVID website.
We’re not seeing nearly as much influenza and RSV as we were a few weeks ago. I did have a patient this week that I was pretty sure had influenza, but the test came back positive for COVID.
There is a new COVID variant on the scene—XBB.1.5 This variant increased from 4% to 41% of new infections during December and is responsible for 75% of new cases in the Northeast. It’s estimated to be about 40% more infective than its next closest strain. It is not yet known if the strain causes more morbidity and mortality than earlier strains, but it’s not believed to do so.
I’ve written about substance abuse and cannabis a few times during these posts. There’s some data published in the journal Pediatrics this week that we can’t ignore. Between 2017 and 2021, reports of children aged 5 or younger who ingested edible cannabis increased 1375%. Case numbers went from 207 to 3054. That’s huge. Edibles look so much like candy, that kids are drawn to it and adults need to do a better job of keeping it out of reach of kids. I remember when Colorado legalized cannabis and a good friend told me about patients he would care for in the ER—it was not uncommon for babysitters to go look for a snack and find a brownie or cookie and then the parents would come home and found the sitter passed out from cannabis. And remember, a cannabis serving/dose is usually much smaller than the part of the brownie or cookie you would eat if it wasn’t cannabis. The data in this article was obtained from the National Poison Data System, which is typically based on calls to Poison Control Centers (PCC) by both hospitals and people in the community. When I talk to the PCC, they get very specific details about the patient and will link the information I provide to that provided by a parent or EMS if appropriate. Not every ER doc calls about every ingestion or poisoning, though I usually recommend that my team call so that the data system is accurate. As laws change, and edibles become more popular, please be careful of where you leave them if you have kids around (or others in the house or may not realize what they are).
Coronavirus is not quite done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike