For most of the COVID pandemic, Dr. Mike Silverman of the Virginia Hospital Center in Arlington posted highly informative, weekly updates from the. He stopped the regular updates on March 11, but now he’s returned, at least for this week, because “There is a lot of news going on,” including “the end of the public health emergency, the end of the ‘pandemic,’ and fentanyl.” Check out his thoughts – as always, very well informed! – below, and thanks as always to Dr. Silverman for posting these.
Friday Night Update from the ER in Arlington, VA
It has been a minute. I hope this post makes it onto your feed.
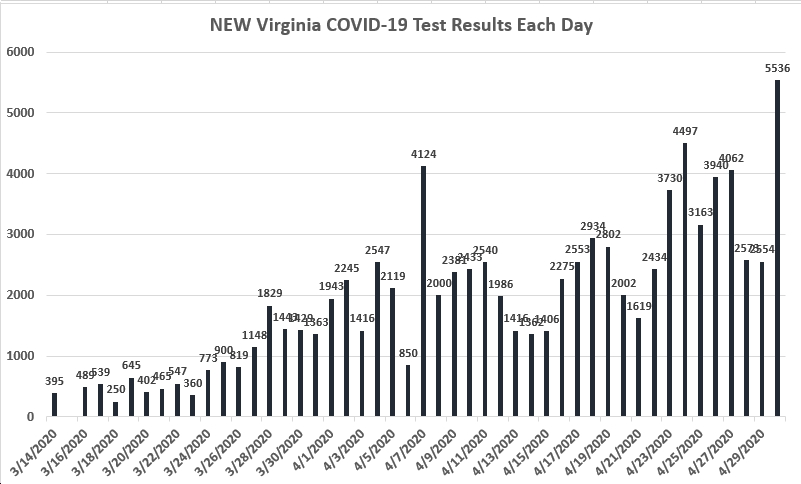
Although we continue to diagnose and treat patients with COVID in the emergency department, our numbers look very good, even compared to my last post 2 months ago. The numbers of hospitalized patients are routinely in the low single digits. The numbers of positive patients we’re diagnosing who are symptomatic also remain in the single digits each week. The total number of patients that we diagnosed with COVID each week also remains about half of what we were getting when I stopped posting on a weekly basis in mid-March. Our percent positive rate remains low as well. I don’t remember the last COVID patient I took care of. It’s been that long.
One of the hot topics in healthcare over the last couple of months had to do with mask requirements in the hospital. Starting in late March/early April, most hospital systems changed their masking requirements. This was in step with CDC data that showed positivity rates less than 5%. Although I have seen a few reports of outbreaks in hospitals, my sense is that is been a relatively smooth transition.
I was on a call this week where hospitals were discussing their rules around masking. It varies based on vaccination status and symptoms as well as patient and provider preference. But essentially all hospitals are trying to be as least restrictive as possible while maintaining patient and staff safety.
You may be wondering why I am choosing this Friday to post. There is a lot of news going on. I get about a dozen emails a day from list serves and medical news sources and I’ve been saving them to remind me of topics to cover. I think I’m up to 150 or so topics I thought would be good to write about. But the real impetus for this week is the end of the public health emergency, the end of the “pandemic,” and fentanyl.
First off, this week (May 11th), marks the ends of the Public Health Emergency (PHE) for COVID-19 in the United States. This means many things including how some of the data will be reported and displayed publicly. Closer to the emergency department, ending the PHE could result in millions of people losing Medicaid coverage. This will translate into patients not being able to get care that is best addressed by primary care or specialty provider. Many of these patients will end up in the emergency department because of lack of access to care or because of untreated illnesses or injuries getting worse. Additionally, while boosters and medications like Paxlovid will likely be covered by insurance, those without insurance may not be able to afford these treatments since they are no longer federally funded. This creates further health inequity.
Last Friday, the World Health Organization (WHO) declared the end to the COVID 19 global health emergency. The International Health Regulations Emergency Committee met on Thursday, May 4th, and stated that the “public health emergency of international concern that started with the coronavirus outbreak in January 2020 should end.” This does not mean that COVID infections are not a currently occurring or that the virus has disappeared from existence. However, it does mean that the WHO official believes that the coronavirus is a lower level of concern. There are still more than 10,000 people a day hospitalized with COVID in the United States and over 150 people a day dying. However just like our data at the hospital shows, the numbers are significantly improved to even a couple of months ago.
The CDC also made changes to booster recommendations as of May 1. An additional shot of the bivalent booster has been approved for those over 65 or are moderately or severely immunocompromise. People who previously received bivalent vaccine have an option to receive an additional dose as well. There was a big study out of Canada published earlier this week. Researchers looked at 1.5 million hospital admissions during the first 2 years of the pandemic. Unvaccinated patients were found to be 15 times more likely to die than fully vaccinated patients. The study period was from March 2020 2 May 2022. Scientist even found that during the fifth and sixth waves, roughly from late December 2021 to March 2022, this is after the full vaccine rollout, “the proportion of adults admitted to the ICU was significantly lower at 8.7% compared to 21.8%” between vaccinated unvaccinated patients. In these later waves, even when more and more vaccinated patients required hospitalization because the prevalence of the disease increased in the community, the authors show that the COVID cases tended to be less severe among the vaccinated patients. At the end of the day, vaccinations were beneficial to protecting against severe disease.
Tuesday May 9th was the second annual National Fentanyl Awareness Day. This day of observance was founded by parents who lost loved ones to the drug overdose crisis. The aim of this days to “raise awareness that people were dying at alarming rates due to illegally made fentanyl, a dangerous synthetic opioid.” Fentanyl is 50 time stronger than heroin and 100 time stronger than morphine. There is a growing threat in the United States and even a small dose can be deadly. There is an emerging threat that fentanyl is now being mixed with xylazine, and animal sedative, which makes it even deadlier. “The age-adjusted overdose death rate involving fentanyl rose by 279%, from 5.7 per 100,000 standard population in 2016 to 21.6 per 100,000 in 2021, as reported by the CDC’s National Center for health statistics. Rates of overdose deaths from heroin fell by almost 41%. Males are much more likely to overdose than females. When I worked in Baltimore City, it was not uncommon to give Narcan for heroin overdoses on a daily basis in the emergency department. Now when I talk to my colleagues there, they say essentially all of the overdoses are related to fentanyl and they are no longer seeing heroin. Interestingly enough, our standard urine tox screen detects opioids but until recently, did not separate out fentanyl. In fact, many hospitals do not have the equipment at this time to detect fentanyl. However, this is changing and we’ll see if identifying fentanyl as the agent that led to the overdose has a clinical impact. I do believe that with the right infrastructure, the data can influence the tracking of fentanyl use and/or overdose.
Closer to home, this week we’ve had some tears and some celebrations.
We lost our long time night shift doc this week to a battle with lung cancer. Dr Griswell was a larger than life man, affectionately known as Dr Gris or Gris, who started working nights at VHC in 1989. He worked a ton of hours by anyone’s standards and was always happy to be at work. When COVID hit, he was certainly old enough to retire and as a former smoker, had concerns about his own risk (and all of us worried about his health as well). Despite that, he decided to continue working so he could be there to help people. In 2010, he went to Haiti after the earthquake because he knew people needed his help. Team Rubicon leader Jake Wood (see link in comments) posted a great story yesterday of how he met and then worked with Gris that you can find on Facebook and Instagram. I highly recommend finding it. If you came to our ER in the last 30+ years, you had at least a 25% chance of having Gris take care of you.
On a more positive note, we recently celebrated nurses week and hospital week. One of the benefits of being the emergency department chair is being invited to our hospital’s Friends of Nursing and Healthcare Awards reception, held earlier this week. We have great nurses in the emergency department who always are well represented among the award recipients and nominees. Nursing is the foundation to high quality providing care in the ER. The profession requires the right mix of strength, endurance, empathy, compassion and toughness. We have a great team that are also fun to work with. Please see the attached picture.
Finally, congrats to my daughter who graduates college this weekend with a double major in computer science and math. She definitely takes after her mother.
Coronavirus hasn’t disappeared, yet we’ve learned to live with it.
Science matters.
Mike