Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
Thank you so much to everyone who left their locations for me last week. It’s unbelievable to me how this post finds it’s way around the world. From the Philippines to Russia to multiple countries in Africa to Australia and New Zealand. Within the US, it’s also really fun for me to see the cities and states where readers are. Many of you are connected to some friend of mine, but there’s probably more who have come across this though people I don’t know. I really was touched by the comments, and they certainly inspire me to continue writing these posts.
My posts have been short the last couple of weeks. This one may require that second drink tonight or a second cup of coffee if you’re a Saturday morning reader.
About 680,000 Americans have died of Covid since it began in 2020. According to Johns Hopkins University, “average deaths per day have climbed to 40% over the past 2 weeks, from 1387 to 1947.” The overwhelming majority of the deaths are occurring in the unvaccinated. Our current 7-day average is just over 2000 deaths per day. We are starting to see a slight decrease in the national 7-day average of new cases. This is huge. The average daily deaths should also start to go down over the next few weeks. As a country, we’re quite possibly over the hump of the current surge.
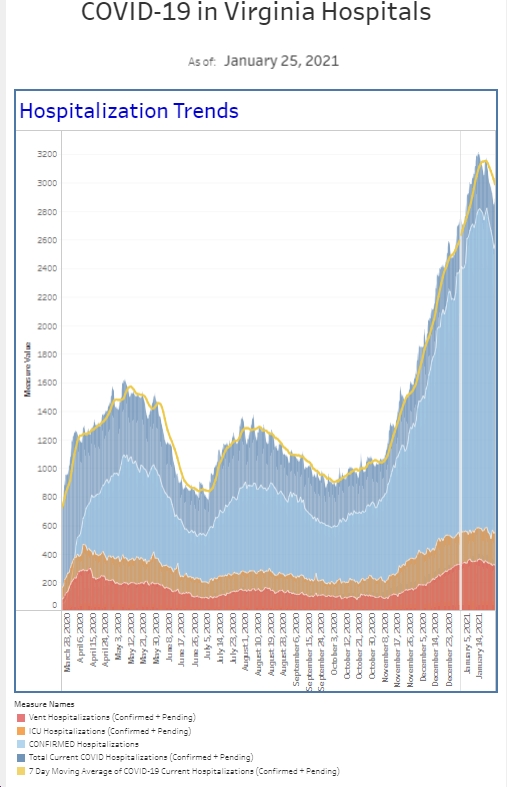
While we’re seeing a decline in new cases nationally, locally is just a little bit different. The ER site is quite interesting. Our volume and acuity is the busiest it has been since the pandemic started. For that reason alone, I expect to see increased testing and an increase in the number of positives. For starters, we performed the most rapid COVID tests in 1 week that we have ever done. And I’ve tracked this metric since April 2020. We also had the highest number of positive tests among all patients since the week of March 3rd of this year. We had about 50% more positive tests than we have had the last 2 weeks. This is also the highest number of positive cases among our symptomatic patient population since March as well. Looking at our patient population that requires “covid isolation,” we saw an increase in the number of patients who met are criteria and in increase the number who required admission, with numbers similar to what we saw last spring. The hospital inpatient census actually picked up a good bit this past week. Is perhaps within normal week to week variability, but there is more patients requiring hospitalization there I can recall the last several months. Our inpatient census bump is pretty consistent with national trends as well, as hospitalizations increase a few weeks after cases increase.
There are days when I am walking into the hospital and putting my mask on, I think to myself, “holy cow I cannot believe I am an ER doctor in the middle of a 1 and 100 year pandemic.” Then I tell myself, “we have been doing this for over 18 months, nothing is new, you should be used to it.” Realistically, I may cuss when I talk to myself. We are still knee deep in Covid, but there is a lot of positive news this past week, including the decline in new daily cases and approval of boosters for many high risk patients, and that gives me a little bit of optimism. (Shoutout to HM who didn’t think that word was in my vocabulary).
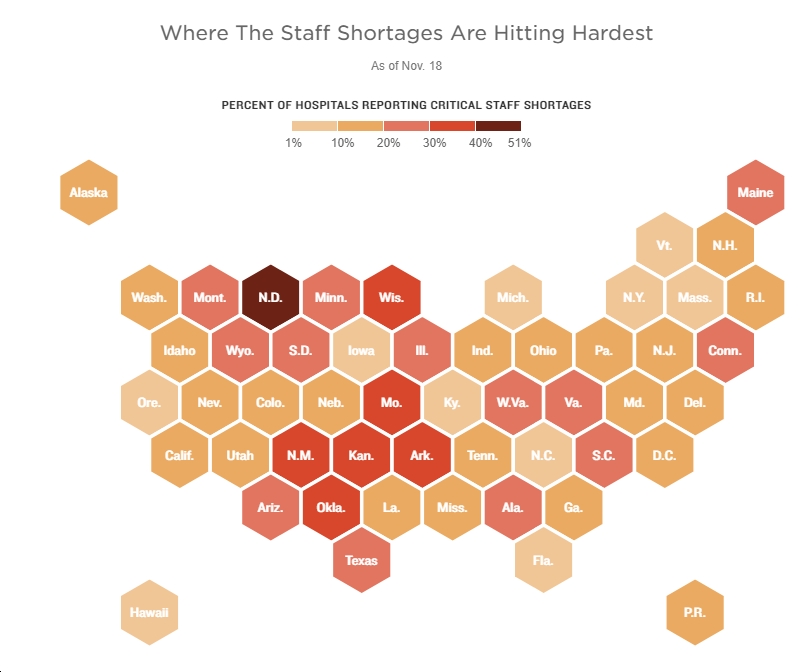
The FDA approved a 3rd dose of the Pfizer vaccine (6 months after your second Pfizer dose) for those 65 and older, those at high risk of severe disease (a broad category), and people whose jobs put them at risk of infection. This then went to the CDC’s Advisory Committee yesterday for final review before approval by the CDC Director. The Advisory Committee recommendations were a little different than expected but will cover about 10% of those previously vaccinated with Pfizer. While the CDC recommended those 65+ and those in long term care facilities, they did not recommend boosters for healthcare workers (and others like teachers) who are at high risk from an exposure point of view. Personally, thatwas pretty disappointing to me as our staff remain at risk. Staffing shortages exist and even asymptomatic infection will take workers out of the hospital for 10-14 days. However, the CDC Director disagreed with her panel and brought back boosters 18-64 year olds at high risk jobs or institutional setting (healthcare workers, teachers, those in prison or homeless shelters). Other recommendations included boosters for those 50-64 with underlying disease and a recommendation that those 18-49 year olds with underlying disease consult with their physician first to weigh the risks and benefits, but are allowed a booster if recommended.
I don’t know how much of the CDC’s decision to not offer boosters to everyone after 6 months is politics versus science, but with 182 million Americans fully vaccinated, operationally the nation needed to find a way to phase people into the booster group. There’s also tremendous international pressure to not give boosters to everyone when so much of the world still needs their first shot. For example, less than 4% of Africa’s population is fully vaccinated. Finally, there’s still a lot of Americans who need their first shot as well. I anticipate that vaccination recommendations will change over the next couple of months, particularly as Moderna and J&J bring data to the FDA (more on that shortly).
There is an interesting study looking at healthcare workers and the risk of infection published in the NEJM this week, involving 5000 healthcare workers across 25 states. Participants underwent biweekly testing and vaccination with Pfizer and Moderna were found to be 88% and 95%, respectively, effective in preventing COVID. Of course, the study only went out 14 weeks and concluded before Delta was the predominate variant, but it’s a good start. There was also a drop off in effectiveness after 8 weeks. Although I’m pretty good about PPE at work, I am happy to get a booster.
Lost in the booster news last Friday was the CDC MMWR’s report comparing vaccine effectiveness between Pfizer, Moderna, and J&J in patients who are not immunosuppressed. The study looked at patients from March to August in preventing hospitalization. This was a case control analysis with almost 3700 patients among 21 hospitals in 18 states. Vaccine effectiveness against COVID hospitalizations was best for Moderna (93%). Pfizer was 88% and J&J was 71%. The Pfizer vaccine did see a drop off in effectiveness 4 months after the second shot and this is why we’ll continue to hear about Pfizer booster recommendations. Moderna’s success is also why they may have trouble getting boosters approved except for certain subgroups. Although there are some differences in the results, the authors concluded that all vaccines “provide substantial protection against hospitalization.”
J and J released data on their booster, which indicated a second shot at 2 months increases efficacy from 79 to 94% against symptomatic illness. I don’t want to rain on anyone’s parade but the international arm of the study showed a 75% efficacy so I think we’ll know more when they release all the data. And don’t’ fret if you got your initial dose more than 2 months ago as J&J is saying that if you get the booster 6 months later, it’s even more effective. They’re reporting 100% effectiveness in reducing severe disease (hospitalization and death). Don’t rush to schedule your booster yet as they need to submit data to the FDA and go through the same approval process that Pfizer is doing. But it’s good news and really the first news we’ve had in a while.
Let’s catch up on some data from two weeks ago looking at vaccine effectiveness. I briefly got into this last Friday but want to really be clear about the details. The CDC released data from 600,000 cases in 13 states from April to mid-July. Unvaccinated people were 4.5 times more likely than vaccinated to get infected, over 10 times more likely to be hospitalized, and 11 times more likely to die. That’s pretty compelling evidence that the vaccine works really well to protect you from severe disease and death, and still works to reduce your risk of infection. Most of the data I see hospitals post demonstrate that only about 10-15% of hospitalized patients with COVID are vaccinated. And the unvaccinated make up larger percentages when you’re talking about ICU beds or requiring mechanical ventilation. Boosters will further reduce the hospitalization numbers for the vaccinated.
“Since July, the pediatric cases of COVID 19 cases have increased by about 240% in the US,” said the Pfizer CEO earlier this week as Pfizer released some safety and immunogenicity data from their studies on about 2300 kids <12 years old. They have not applied for Emergency Use Authorization for 5-11 year olds yet but it’s coming soon. We learned about dosing and immune response. The standard dose for 12+ is 30 micrograms (ug) and for the study they looked at 10 and 20 ug doses, in addition to the full 30 ug dose that has been used for 12+. The antibody response at 10 ug for <12 compared favorably with the response in the 16-25 year old age group. Pfizer also announced that they expect to have data to submit for 2-5 year olds and for those 6 months to 2 years later this year.
There was an article that appeared in the Atlantic magazine on September 13 discussing the types of patients being admitted to the hospital. The number of patients that require hospitalization has been an important metric throughout this pandemic. It is important to understand what types of patients are being admitted and to make sure that appropriate patients are in the hospital and patients that do not need to be in the hospital are not admitted. This is critical because hospitals appear to be busting at the seams, ICUs are overflowing, and we continue to hear about patients not being able to get the care that they need, whether this is related to a particular surgery or an ICU bed. Researchers from well-respected academic institutions published a “short report” online looking at patients admitted to a VA hospital with lab confirmed COVID. They compared the pre-vaccine and post-vaccine admission acuity defined as oxygen levels less than 94%, which would require additional oxygen. (Honestly, many hospitals are going as low as 88-90% as a threshold because bed capacity is so limited) The authors looked at over 47,000 admissions across the VA population. Prior to the vaccine, about 64% of Covid admissions were defined as moderate to severe. After the vaccine, this number decreased to 52%. The results show that “disease severity in the vaccine era among hospitalized patients was lower among both unvaccinated and vaccinated patients.” One of their conclusions was that there may need to be some other measures of disease that define moderate and severe Covid which would aid with tracking. As a clinician, thinking that half of the patients we admit with Covid are arguably not sick enough to be in the hospital, does not pass the sniff test with me. It’s possible this is because there are differences in my community patient population versus a VA patient community.
Here are a few examples. The schizophrenic patient who was brought in because they are having worsening delusions, thinking that their family is trying to kill them. Over and over, we saw that these patients had Covid and had lost their sense of taste and smell which exacerbated paranoia and delusions. Explaining to patient’s the etiology of this does not prevent their need for psychiatric admission. Example two, the elderly patient who tripped and fell and broke thier hip secondary to weakness.
Again, over and over, these patients would come back as Covid positive which was the cause of their general weakness which then led to their fall and hip fracture. We also saw many elderly patients who also lost their sense of taste and smell and stopped eating. These patients were Covid positive, may not have had pneumonia, but came in for severe dehydration and electrolyte abnormalities that requird admission. Finally, there are patients who may not be hypoxic enough to require oxygen immediately, but are breathing rapidly and have a rapid heart rate. Some of these patients get admitted for monitoring because we anticipate that they will not be able to keep up with her breathing demands and ultimately require oxygen.
This is the case more often than not. Over and over, ER docs around the country are sending home patients with COVID safely despite having vital signs that we typically would have admitted someone for prior to COVID. While I think this is an interesting study, and likely shows the benefit of vaccines giving us patients that are less sick compared to the pre-vaccine setting, it does highlight that COVID is more than just an oxygen saturation number at triage when decisions are made about admission. Other vital signs and laboratory values should be added to the definition for mild and moderate COVID related disease.
And a very happy birthday to my wife. We’ll be getting Mexican food tonight to celebrate.
The picture is from pet therapy time for the ER staff this morning. It doesn’t occur often enough, but I was glad to get some dog smooches this morning at work.
Science matters. Get vaccinated. Wear a mask. We’re not quite there.
Mike