Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
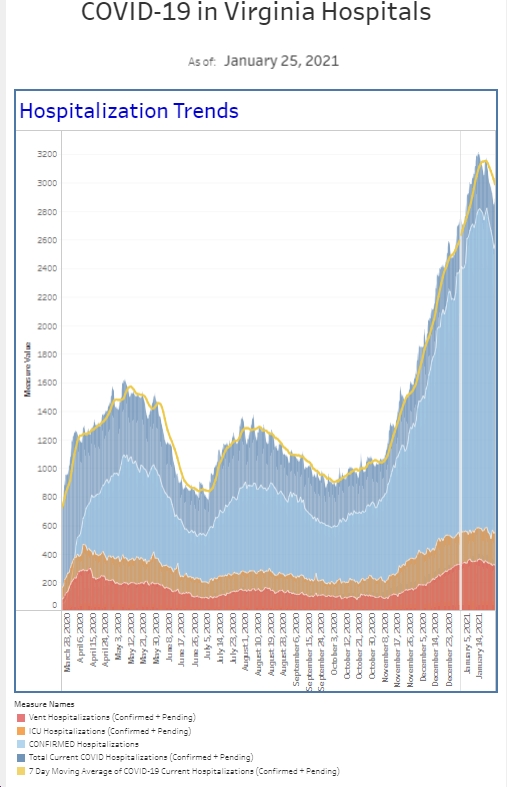
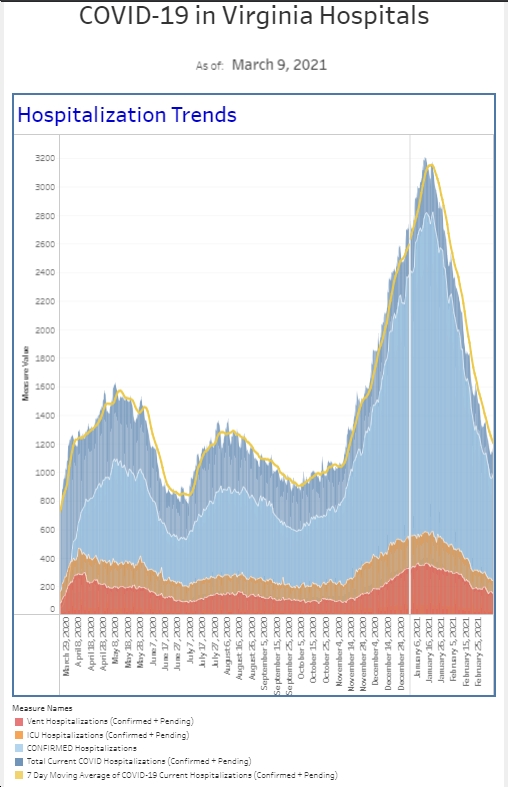
As I look around the emergency department and the hospital, we are in pretty much the same place we were last week. Our hospital census (the number of patients hospitalized with COVID) is basically the same. The number of tests we performed among our “symptomatic patients” was the same for the last two weeks, though this week, there is 1 less positive test, resulting in a slight decrease in the positivity rate. But 1 out of about 110 tests performed, does not seem like a big improvement. We did actually have a noticeable decline in positive tests among our asymptomatic patients. We are still seeing positive tests in this category of patients, but if you are looking for good news, a drop in this positivity rate is good. The number of patients who require our COVID isolation status (either as a known positive or prior to testing) has been pretty stable for the last 6 weeks. It’s about twice the number we had each week in July but fortunately has not increased as dramatically as other surges. As I look at the data that I started collecting in March 2020, the trends the jump out at me are the 10 to 12-week cycles where we see dramatic numbers of cases increase, peak, and then decrease, before falling off to a new steady state. With that in mind, we are probably about 6 weeks into our current surge without the steep slope upwards. And more good news is that our current surge is less than about half the number of positive cases and half the number of patients requiring COVID isolation than we saw in the winter surge.
Now that the real business is out of the way, this is going to be brief tonight.
Last weekend was my summer holiday weekend to work. So, I am at the end of a pretty long 2-week run. I am tired.
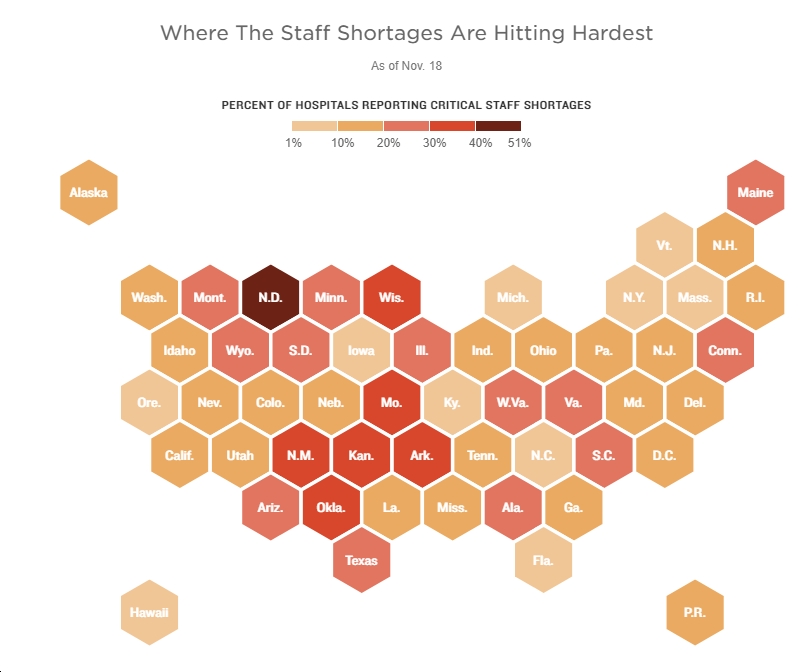
I do not talk a lot about how healthcare workers or I, specifically, feel regarding the fatigue or frustration we have with what’s going on around the country. People are protesting outside of hospitals, making healthcare workers feel unsafe. People are refusing to believe experts and science. People are creating their own reality. This week, the American Nursing Association asked the government to declare the nursing shortage as a national crisis. When we talked about flattening the curve 18 months ago, it was about protecting hospital resources. Nurses (and doctors) as well as all the other people that make the hospital function properly, are tired. The nursing shortages are real all over America. They will get worse the longer the pandemic goes on. We need to reduce cases to protect the future of hospitalized medicine, not just cases related to COVID.
I am a little young to really remember the Vietnam War. What I believed when I was younger (and still believe to be true) was that soldiers were sent there for a year and would expect to go home after 12 months. I used a little bit of the mentality of “I can do anything for a year” and it’s way better than being in a war, to help get me through med school and residency. I loved med school and residency but it was hard. Internship had many months of working more than 120 hours a week and 2 months in a row of working more than 140 hours a week. But I knew at the end to 12 months of internship, it would be over and my life would get better (at least the staggered every other night call was behind me). I think it is very hard for a lot of people on the front lines of healthcare to see a real end to the pandemic and to find a break with all that’s going on. Covid is likely to impact us in the hospital for the next couple of years. We need to start working on protecting our vital resources. Certainly, increasing vaccination rates and decreasing the morbidity mortality associated with Covid will help with that.
I want to touch on a couple of things out of the CDC recently. There was a study comparing state level pediatric ER visits and hospitalization rates comparing June to August (pre-Delta to Delta) and not surprisingly, found an inverse correlation between increases in ER visits/hospitalizations and a lower vaccination rate for those 12 and older. Higher COVID issues correlated with lower vaccination rates. If your state was in the bottom 25% of vaccination rates among states, the state had about 3.5 times more ER visits and hospitalizations compared to states in the top quartile.
Why else are vaccines important? There was an outbreak last spring in Marin County, CA. Elementary school students were exposed to one unvaccinated and infected teacher which led to a 50% infection rate in one classroom. Eight of ten students in the front two rows were infected and 4 of fourteen students in back three rows (proximity matters). Including contacts in other grades and family members, 27 people were infected.
School is now in full swing throughout the area. While I’m not aware of any new cases at my son’s school (trust me, I’m knocking on wood right now), I’ve had a handful of colleagues tell me about infections that have come up at their kid’s schools or daycare.
We need everyone to get vaccinated if you’re >12 years old. The younger kids will get approved soon (hopefully by the end of the year).
Science matters. Get vaccinated. Wear a mask. We’re not quite there.
Mike