Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
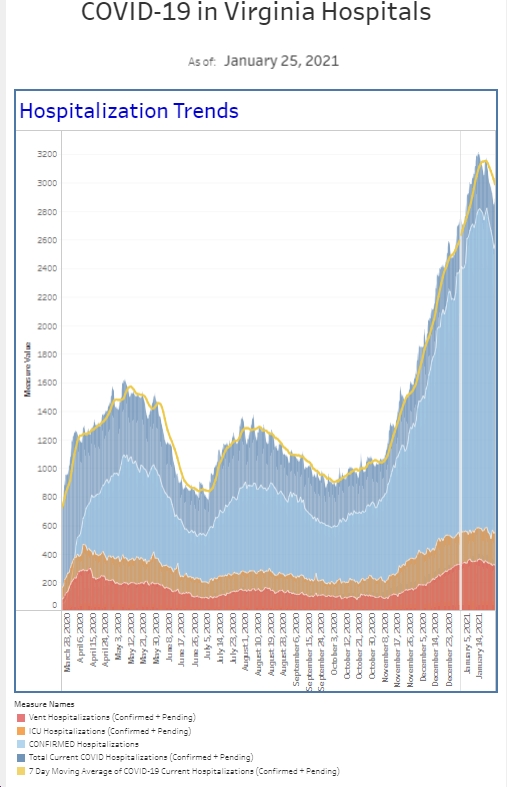
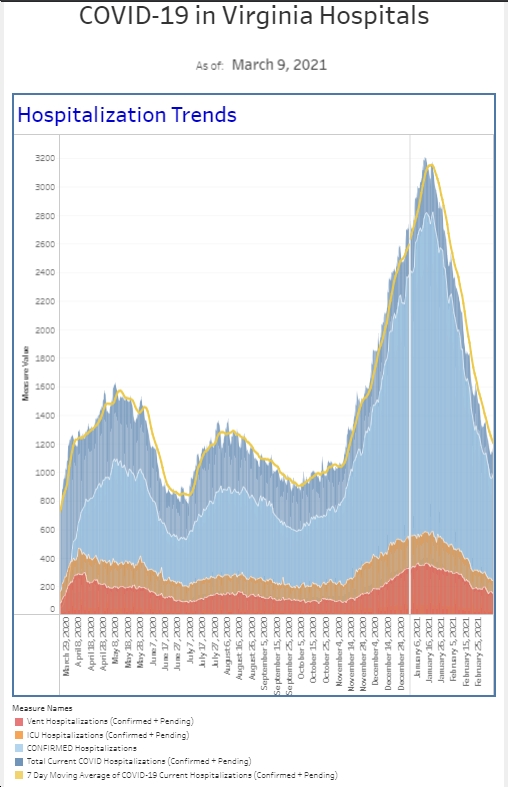
We definitely had a decrease in the number of Covid patients we diagnosed in the ED this week, seeing the least amount among our symptomatic and asymptomatic patient populations since late July. This corresponded with a drop in the percent positive rate, well below our running 6-week average in each patient population. We also had a noticeable drop off in the number of patients who required our COVID isolation protocol. This is all welcome news. The hospital census has not seen a decline yet, but if our trends in the ER keep up, I expect a drop in the hospital census over the next couple of weeks.
We have all seen different shortages as a result of the pandemic and the issues related to the global supply chain. We certainly had our share in healthcare early on, but things have been relatively stable over the past year. You may be aware of the plastic shortage currently going on now. My household started to feel this about a month ago when we could not find Lunchables, a lunch mainstay for our son (no judgement please). We are now feeling that shortage of plastics here in the hospital. There is a critical shortage of pretty much everything having to do with IVs, from the actual IV itself, to the connector we used to hook it up to IV fluids, to the saline flushes, and the bags of fluids. IV fluids are a mainstay of treatment, particularly in patients with sepsis, where we are more aggressively giving IV fluids now than we were a years ago. We dealt with a saline fluid shortage several years ago when a manufacturing plant was severely damaged during a hurricane. The healthcare system responded, and we found ways to reduce IV fluid use but I’m not sure there’s a lot of low hanging fruit left to pick when it comes to reducing IV utilization. While we are not out of supplies yet, unless the healthcare systems across the board find alternatives and/or begins restricting usage, it is certainly in the realm of possibility that we could run out before our next shipment comes. The majority of patients who come to the emergency department end up with an IV and fluids. However, a large percentage of these patients do not need them, and this will be one of those additional discussions that will need to take place in ERs around the country so that we can preserve our resources for the patients who truly need them.
There was a very interesting study released this week in preprint form (not peer-reviewed yet). The authors prospectively looked at 8.8 million New York adults, and compared vaccinated groups by the type of vaccine, month of full vaccination, and patient’s age to unvaccinated age specific cohorts. They then examined statewide databases to evaluate vaccine effectiveness against getting Covid (particularly related to time after full vaccination) and vaccine effectiveness to prevent hospitalization. Again, Moderna performed better than Pfizer and Johnson & Johnson in preventing Covid over time but all products had a decline in their effectiveness over time. Vaccine effectiveness against hospitalization held up pretty well among all 3 vaccine, though again Moderna performed better than the others. There is more decline in vaccine effectiveness preventing hospitalizations in those over 65 which the authors say supports giving booster shots to that age group.
The FDA advisory panel has been meeting the last two days and recommended a half dose booster for Moderna patients. Although Moderna has held up very well, scientists presented data showing that people vaccinated more recently were less likely to have breakthrough infections compared to those vaccinated longer ago. The advisory committee recommendations for boosters are similar to those who can get a Pfizer booster and are focused on reducing hospitalization and death risk, not necessarily on preventing infections. The groups include those 65 and older, those 18-64 who have underlying disease putting them at higher risk of severe COVID, and those whose occupations or living situation put them at risk for severe disease (nursing homes, jail, healthcare workers, teachers, etc). The next step is the CDC meetings next week but I suspect Moderna patients will be able to get boosters soon.
Another interesting article that came out this week looked at mixing and matching booster shots with the original vaccine. NIH released a pre-print study looking at 458 individuals (relatively small number but a good start) who had been vaccinated with Pfizer, Moderna, or J and J, and then got a booster injection at least 12 weeks after the initial vaccine series with one of the three. This 3 x 3 grid leads to 9 combinations. The end result at day 29 was that mixing and matching vaccines is safe, well tolerated, and leads to an improved immune response in a lab setting. You would need a much bigger study to look at real life vaccine effectiveness, but this is a good start.
The FDA considered the J&J booster today as well. J&J isn’t about waning immunity, but rather increasing efficacy and the FDA advisory panel recommended a booster 2+ months after the first injection for those 18 and older, which covers a broader age group than Moderna and Pfizer. The hope is to reduce the number of breakthrough infections which occurs more commonly with J&J than the others. J&J brought data for boosters ranging from 2-6 months. The big question not being answered yet is whether eventually there will be a formal recommendation to allow mixing any booster regardless of the primary vaccine. The FDA did not vote on this today. I know many people got a mRNA booster as a “first dose” 6+ plus months after receiving a J&J primary vaccine. Hopefully the FDA and CDC will weigh in on the safety and efficacy of this combination at some point as the data seems pretty good.
As a doctor, I am pretty good at taking a clinical approach to patients. However, as a husband, father, and individual, sometimes I act the role and worry about worst case scenarios. As a parent, and an ER doctor, I have been known to tell my kids after they fall that if they do not have a bone poking through skin, they should just get up and wash it off and go back to playing. But I also worried about the one in a million chance my son would get myocarditis after his covid vaccine. I asked him about chest pain a couple of times even though I knew the actual risk was incredibly low. With that said, I got my booster shot the other day before my shift. Hypothetically, my 15 minute observation period was going to take place in the ER as I worked. As I walked back to the ER after the shot, I did have just a second of panic about what would happen if I had an allergic reaction in the hospital corridor. I also wondered how crummy I would feel by the end of my shift. It was a tough shift and I started to get a headache by the end. By this point, I really had not eaten in about 10 hours which is not unusual during a shift. I was not sure if I was hungry, tired, or if the booster messing with me. Fortunately, some good greasy food at the end of my shift made me realize it was just hunger.
The next day, my son texted me from school to say he was sick and would need to come home. He said he was too sick to play his soccer game that day, so I knew it was real. This was the first time anyone in my immediate family has gotten sick in the last 2 years, and I was really wondering what I would do to get him tested. I had been in CVS and Walgreens earlier this week just looking to see if I could pick up a couple of over-the-counter rapid tests. Both places told me that they have been sold out for ages. It’s really crazy to think that 18 months into this pandemic, getting a rapid test can be so difficult.
About 10 days ago, the NYTimes reported that Biden planned to invest $1B to increase the supply of rapid, at home (antigen) tests, quadrupling the supply by the end of the year. This can’t come soon enough in my mind. Back to my son. As it turns out, my son’s school nurse does testing, and his rapid test was negative but he could not go back until his PCR test comes back negative. (he’s negative and doing better, thanks!) We also got a sick appointment at the pediatrician that afternoon. I was really impressed the school nurse did testing (huge help) and also impressed with how the pediatrician’s office pivoted during the pandemic to provide drive-through testing as well.
As I said last week, I got my flu shot and hopefully you have a plan to get your flu shot as well. I want to provide data on what happened to flu since the pandemic started, and give a huge shout out to Val, our administrative director of pathology. I asked Val what I thought would be a fairly simple big picture question about flu testing here at the hospital and got a very elaborate and detailed answer. Flu has all but disappeared since COVID arrived—you can thank masks, social distancing, hand hygiene, and flu vaccinations. We have seen 2 cases of flu here in the last 2 months. That’s a touch below our typical for August and September but it’s reassuring to know that flu is not widespread yet in the community and you have times get your flu shot. Influenza, the flu, generally occurs in the fall and winter, and typically peaks between December and March. ER docs often make the diagnosis of flu based on the clinical history and physical exam. Prior to COVID, unless you’re very young, old, being admitted, or pregnant, if you go to emergency department your you may or may not have gotten a flu test. The rapid flu test is not a great test and often gives a negative result when in fact the patient has the flu. (We do have a very expensive PCR virus test that can help identify about two dozen specific viruses but it’s so expensive, we generally don’t use it routinely on patients who do not require admission).
Although the flu test is not great, we do typically order it over a thousand times a month during the fall and winter. This does allow for some consistency in tracking lab documented positive tests and allows us to see percent positivity rates. Looking at data in the 2 winters prior to Covid, specifically 1st quarter 2019 and 1st quarter 2020, the hospital lab ran thousands and thousands of flu tests with a percent positive rate of about 15%. Compare that to the first quarter 2021 when we ran approximately 1800 flu test and had only one positive. Our patient volume was a lot lower first quarter 2021, but we still were clinically suspicious enough to test a lot of people for influenza. Let’s look at a little more data. We do not usually have a lot of positive flu test in the second quarter of the year however in both 2018 and 2019, our percent positivity rate was in the 5 to 6%. Everything really shut down in the second quarter of 2020 and we had 0 cases that quarter. That’s a 0% positivity rate. Nevertheless, look at 2021 when things started to open up, as many people had gotten COVID vaccinated, we also had an extraordinarily low number of positive cases with a positivity rate of 0.2%.
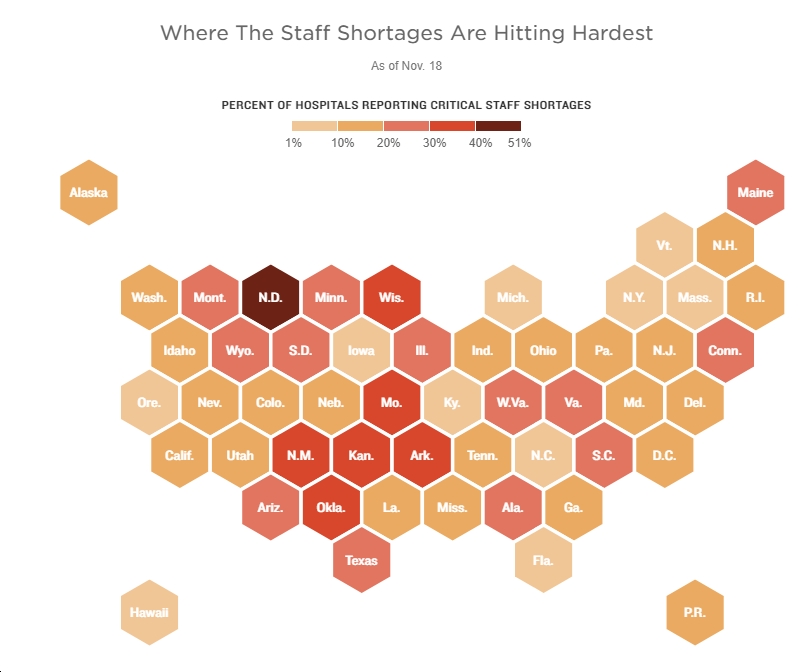
So why are the numbers so low? If you recall last year, there was a huge push for people to get their flu vaccines because you did not want flu and COVID at the same time. There was also a tremendous amount of social distancing going on and mask wearing because COVID was so bad. I do not anticipate that we will have the same amount of social distancing and mask wearing this flu season as we had a year ago. All of this is to say, get your flu shot. Protect yourself and your family. Although COVID is slowing down now, it’s certainly possible we will see another winter surge. The healthcare system is still busting at the seams. Increases in patient volume and acuity if both flu and COVID pick up, will present extraordinary challenges.
Flu risk (and COVID risk) will increase as I expect people to try to plan holiday get-togethers this year (hopefully safely). I am working Thanksgiving Day but do expect to see my extended family over that holiday weekend. There are certainly ways to do these kinds of events safely, particularly if everyone is vaccinated and asymptomatic.
It’s the end of Emergency Nurses Week. If any group deserves to be celebrated this year, it’s these professionals who have been on the front lines of the pandemic since day 1.
They’ve seen it all—volume and acuity shifts, staffing challenges, young and old dying, and more. They are there to start your IV, adjust your oxygen, provide lifesaving medications, hold your hand, and talk to your family. Nurses have saved me many times in my career, made me a better doctor, and help me enjoy my job. I’m incredibly fortunate to work with such a great team and I know we’ll remember this pandemic experience for the rest of our lives. Please take a minute to thank any of the ER nurses in your life (or mine).
Science matters. Get vaccinated. Wear a mask. We’re not quite there.
Mike