Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
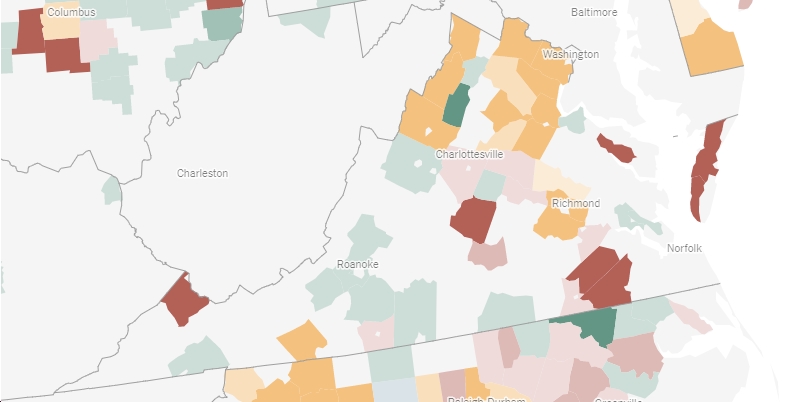
Consistent with the rest of the country and the reports you’re seeing elsewhere, we are seeing an increasing number of COVID patients present to the ER. Numbers wise, this past week we had increasing numbers of “symptomatic” patients present and get tested. Among this subgroup, we saw an increasing percent positive rate going from 7% six weeks ago to 15% this past week. The total numbers of positives are up 4x in that time period. Including our asymptomatic/screening patients, we’re seeing increasing numbers of positives week over week. Overall, we’re performing about 20% more compared to a few weeks ago and across the ER, our percent positive rate went 2% to almost 6% with a 2.5 fold increase in total positives over the last month. One of the differences this go around compared to last winter or summer is the increased number of patients coming in with positive tests from outside testing centers who are now feeling worse.
One way we account for these patients is by tracking the number of our times we use our “COVID isolation” order set. We also track the disposition (admit, discharge, etc) for patients who require this order set. We’ve seen a definite increase in the number of times we use this order set over the past 2 weeks. We’re also seeing an increasing number of patients requiring hospitalization who are covid positive, though the actual percentage of patients in “covid isolation” has not climbed. Looking at our hospital census, it’s grown a lot since last week. Most of the patients who get admitted are not vaccinated.
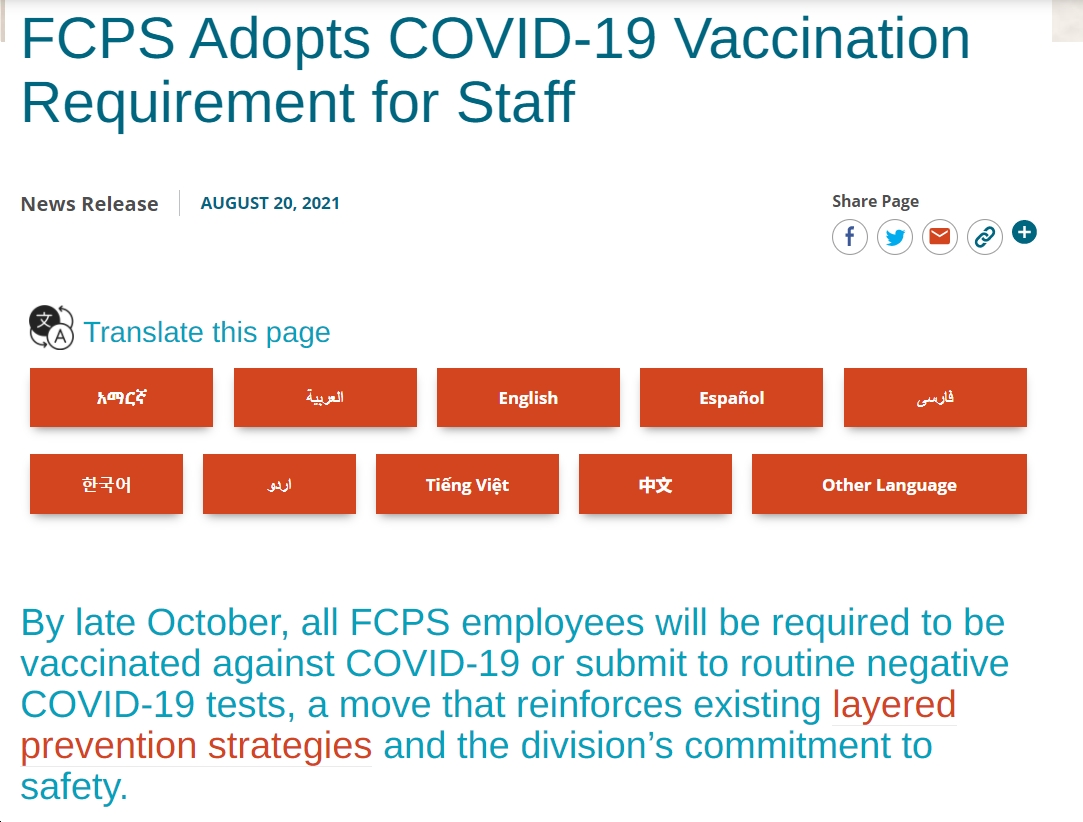
This was a very heavy clinical week for me. I can honestly say that I personally saw more patients with COVID this week than I have in the last 4 to 6 weeks combined. Many of the patients already had been diagnosed. I can usually know what the disposition is going to be from the triage note—age, symptoms, and vital signs go a long way. The first patient I saw this week was critically ill and was admitted to the ICU. He had been diagnosed a couple of days before coming to the hospital. We have known all along that there is a subset of people who will continue to get sicker for several days after they have gotten diagnosed. However, we don’t know who is going to get sicker from the time of diagnosis and require hospitalization. Even some of the young adults I have seen were surprised at how bad they felt, yet they did not require hospitalization. The very sick patients we’re seeing are generally not vaccinated. Most of the patients I am discharging, are vaccinated. It continues to be very simple, if you are not vaccinated, you need to get vaccinated. If it has been 6 months since your second dose of mRNA vaccine, get your booster. Also, if you haven’t already, please buy a pulse ox. They cost about $15-25 and can be used to assess your oxygen level. If your level is below 92%, seek medical attention.
Although vaccinations are still the best way to prevent severe illness, we know that a subset of people will have breakthrough infections despite the vaccines (and boosters). There’s a recent study looking at what groups get hospitalized when they experience a breakthrough infection. Looking between June and September (Delta variant), the Kaiser Family Foundation found almost 70 percent of fully vaccinated patients admitted to hospitals with confirmed COVID-19 were aged 65 and older,” while 10% “of breakthrough hospitalizations occurred among those younger than 50, and one-fifth occurred among those aged 50 to 64.” If you’re young and healthy, the vaccine is highly effective in preventing serious illness if you get a breakthrough infection.
Yesterday was the 1-year anniversary of my first dose of vaccine. Last year at this time, we were heading into the winter surge and we had big expectations for getting COVID under control in 2021. Although much of the year had a return to normal feel, and despite the vaccine being widely available, deaths in the US during 2021 outnumbered deaths in 2020. Approximately 52% of the 800,000 total COVID seen since the pandemic began were in 2021. (2020 had 385,343 deaths attributed to COVID). About 1% of Americans >65 years old have died of COVID. Despite the vaccine and some advances in medical care, we currently have about 2,000 people a day dying in the US.
Scientists recently attempted to quantify the impact of the vaccine and it turns out, it’s been huge. The vaccine potentially has had a staggering impact and I can’t imagine how many more healthcare workers would have gotten sick or died from COVID had it not been for the vaccine. It’s estimated that the vaccine has prevented “approximately 1.1 million additional COVID-19 deaths and more than 10.3 million additional COVID-19 hospitalizations in the U.S. by November 2021.” It’s estimated there would have been an additional 36 million infections. The death rate could have exceeded 21,000 a day, more than 5 times the peak of 4k per day seen in January 2021.
The omicron variant appears to be highly infective. Although the delta variant was accounting for 96 to 98% of all US cases earlier in the month, were seeing the omicron variant grow quickly from less than 1% to 3% over the last couple weeks. In certain areas, the percentage of omicron patients has already reached 13%. CDC modeling shows that omicron could peak with a massive surge over the next month. The health system is already strained. Even if it turns out that the omicron variant has lower morbidity and mortality compared to the delta variant, a subset of these patients will require hospitalization and some will die. We have already had over 800,000 deaths in the US from Covid. That’s just an overwhelming number from my perspective and yet there continues to be people who do not believe that Covid is real or won’t get vaccinated. I really just cannot understand that. Healthcare workers are becoming increasingly frustrated with the misinformation that’s impacting people’s decisions that could help end the pandemic.
A study out of the University of Hong Kong examined the Omicron variant and the human respiratory track. Researchers found that “Omicron SARS-CoV-2 infects and multiplies 70 times faster than the Delta variant and original SARS-CoV-2 in human bronchus” which likely explains why transmissibility is so much more than other variants. However, they also showed that the virus replicated in the lungs slower than other variants which may be why the disease has not been as severe as Delta.
There is some good news on the horizon. Pfizer released more data from its oral COVID-19 antiviral medication called Paxlovid. Among high risk patients, their data showed that the medication reduces the risk of hospitalization or death by 89% if started within 3 days of the onset of symptoms and by 88% if started within 5 days of symptoms. For the groups who got meds by day 3, 0.7% of patients (5 of 697) required hospitalization by day 28. Compared to 6.5% of patients (44 of 682) who received placebo. There were 9 deaths in the placebo group and none in the medication group. There were also no deaths in the group that started the meds by day 5 with about a 1% hospitalization rate compared to a 16% hospitalization rate for placebo. (These patient groups were much smaller though still statistically significant.) Among low risk patients, there was a 70% reduction in hospitalization and no deaths for the patients who receive the medication compared to placebo. Additionally, both high and low risk groups were found to have an approximate 10 fold reduction in viral load. These are from the final analysis of the phase II/III trials. Although this medication looks very promising, you are still better off getting the vaccine and trying to avoid getting Covid.
The CDC has announced their preferred vaccines. No surprise, they’re recommending mRNA vaccines (Pfizer and Moderna) rather than getting a J&J. The effectiveness of the mRNA vaccines are definitely better than J&J and J&J has a higher incidence of blood clots in young and middle aged women. There are no restrictions to J&J but rather the CDC’s Advisory Committee on Immunization Practice has made a “preferential” recommendation.
The Coronavirus is not done with us yet.
Science matters. Get vaccinated (or your booster). Wear a mask.
Mike