Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
We celebrated National Doctors Day this week. Typically, this day is nothing more to me than a slightly fancier lunch that I eat in a different room than the doctor’s lounge at the hospital. And while I am sure I said this last year, my wife always jokes that every day is doctor’s day in our house. (My wife and I also found out this week that engineers get a whole week). All joking aside, I am really appreciative of all the doctors that I worked with throughout my career. I have learned from so many of them and I am so proud of the work that our team does 24/7 at the emergency department and throughout the hospital. It’s been a very difficult two years for everyone involved in healthcare. And while we do not do it for the recognition, (though the notes, cards, and food we’ve received the last 2 years has been awesome), this year I want to certainly say thank you to all of the doctors (and all of the healthcare workers) who have been donning and doffing PPE for over 2 years and altering their work environment and workflow to continue to care for those who need us.
I was saddened to see this week the conviction of a nurse on negligent homicide charges resulting from an error related to medication administration. The nurse now faces prison time. Admittedly I do not know every detail of the case. It’s clear there was a human error involved and a patient died. Typically, serious medical errors are handled through professional licensing boards (for both nurses and doctors) and/or in civil courts, rather than by prosecutors in criminal courts. The nurse, who worked at Vanderbilt, owned the mistake and admitted the error, and ultimately lost her nursing license. For over 20 years, healthcare has tried to break out of the culture of silence by getting people to report mistakes. This leads to the design of better systems and prevents human errors down the line. We’ve all made mistakes in patient care. I can picture exactly how this mistake occurred. I’ve had patients receive the wrong med before. But the approach for reducing human error has to involve finding a system solution. Prosecuting someone for human error is likely to contribute to people being afraid to come forward, which does not improve patient safety. The American Nurses Association has come out strongly about the impact of “criminalization of medical errors” and are in favor of timely reporting, review processes, corrective actions, and system improvements to “preserve safe patient care environments.”
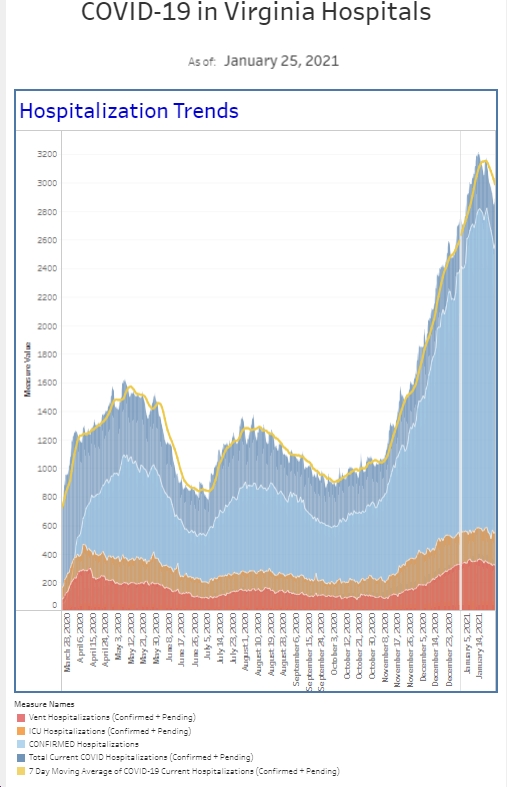
The CDC estimates that the BA.2 variant now makes up 55% of new Covid patients. It’s upwards of 70% in the Northeast. It turns out that one of the more frequently given monoclonal antibodies is not effective against BA.2, so this may end up having a clinical impact. Because BA.2 is more transmissible than the original Omicron variant, which led to the surge over the winter, experts have predicted that we will see a rise in cases. This was seen in Europe as BA.2 became the dominant strain. The DMV is in the 50% range for BA.2.
We did see an increase in the percent positivity rate among our symptomatic patient population this week. We also had an increase in the number of cases for patients presenting with signs and symptoms of Covid. Fortunately, the total number is still low, but it is the highest it has been in a month. The total number of patients that we diagnosed with COVID this past week was actually down a touch compared to the prior week. We also only have a small number of patients with Covid in the hospital. While we are all keeping an eye on the BA.2 variant, we’re not seeing an impact yet in the emergency department. In looking at community transmission data for Arlington County, we did see an increase in the number of cases per 100,000 population last week. This is up from the prior week as is the weekly percent positivity rate. We’re still in the low level as defined by the CDC overall (which includes hospital admissions and capacity). All of this together is worth keeping a close eye on, but I am not raising the warning flags yet.
More relevant to many of us is that the FDA authorized a second booster dose of either Pfizer or Modern vaccine for people 50 and older who receive their first booster dose at least 4 months ago. People 12 and older who are immunocompromised are also eligible for an additional booster. As I have written about previously, data has been mixed on the true benefits of a second booster. However, it is likely to offer some additional protection in preventing a Covid illness, and it is very likely to offer additional protection against severe illness, including hospitalization and death. It sounds like boosters will be recommended this fall as we head back indoors and towards flu season. If you get a booster now, you probably will need one in the fall as well.
Also on the vaccine front was a report showing the benefits of a Pfizer or Moderna booster shot to the 17 million Americans who receive the 1 shot Johnson & Johnson vaccine. A single dose of J&J provided 24% vaccine effectiveness against a Covid associated emergency department/urgent care visit. However, that rate increased to 79% after the J&J was combined with 1 mRNA dose booster. For those who are fully vaccinated with either Pfizer and Moderna, to include a booster shot, they had 83% effectiveness against an ER or urgent care visit. This study was conducted during the Omicron wave. Protection against hospitalization also increased from 31% for those who had 1 dose of J&J to 78% when J&J was combined with 1 dose of an mRNA vaccine, to 90% for those who received 3 doses of an mRNA and a vaccine. Bottom line, if you received a J&J vaccine, you are better off by getting at least one if not 2 doses of the Pfizer or Moderna vaccine.
Every hospital has a doctor’s lounge. If nothing else, it is typically a place with 24-hour coffee and access to computers to get some work done. Most hospitals also have some sort of food there available to the doctors which ultimately makes the doctors more efficient (they don’t leave the hospital for lunch) which makes the hospital more efficient. The doctors lounge in my hospital is pretty well utilized. For many, it serves as not just the cafeteria and dining area, but also as an office (to use the EMR and make phone calls, as a break room, and a chance to catch up with colleagues. Our conversations run from the mundane like any workplace where we are catching up with friends regarding family or vacation to talking about patient’s and talking about treatments. Through the years, I have learned so much from other specialists by having casual conversations about patients or disease entities. Not surprisingly, over the last couple of years, we have also spent a lot of time talking about COVID. I mention all of this because some of the topics that have come up recently include outpatient management for Covid—the new meds are nowhere near as easy to prescribe as the news would lead you to expect–and vaccines. The new medications only have emergency use authorization for a subset of patients who meet certain clinical criteria. Paxlovid, which is the safer of the two, also has a lot of medicine interactions that need to be reviewed prior to prescribing the medication. Some medicines will need to be stopped. Other times, the dose of the Paxlovid needs to be reduced. The primary care doctors definitely seem to be more geared towards prescribing this because they know your past medical history and generally have a pretty up-to-date list of your medications. It is amazing to me how many emergency department patients do not know the names of their medications. Without knowing exactly what medications people are on, it’s obviously much trickier and riskier for an emergency physician to prescribe this medication.
Every doctor that I interact within the doctor’s lounge has received their vaccine and booster. But it is interesting to hear the discussion about who may or may not get a second booster in the immediate future. Some of the docs consider themselves very low risk to get Covid and think there may be a better option in the near future. Therefore, they are comfortable waiting for a more specific vaccine. They are also comfortable getting Covid and recognizing that their risk of severe illness is relatively low. My personal sense is that as an ER doctor, I am more likely to encounter a COVID patient than many other specialties. Because our COVID rate has been low, I am generally wearing just a surgical mask and not an N95. (I do put on the N95 for patients where I suspect COVID or have COVID. Although I am hoping that a vaccine that has been altered to fit the new genetic modifications of the more current variants is out in the near future, I am not so sure that it will be available in the next 3 to 6 months, so I figured I am better off getting the added protection now. (I have not gotten it yet but expect to do so soon). If vaccines are recommended in the fall, I’ll get another. The side effects haven’t been bad for me, so I’m good with 2 boosters in a year if needed. If you only want one shot, maybe wait until fall, since rates are low now and you can spend time with friends and family outside.
I really cannot believe I am still talking about Ivermectin, but there is a great study I feel needs to be mentioned. Published in the New England Journal this week, was a double-blind placebo controlled 1300 patient study out of Brazil that looked at the impact of Ivermectin on patients with mild Covid. No outcome metric was better in the group treated with Ivermectin then with placebo. For those of you that are still hanging onto the believe that this drug helps, this is further evidence that there is no role at this time for ivermectin in the treatment of Covid patients. And I’m thinking we can stop talking about Ivermectin.
The Coronavirus is not done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike