Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
Although it was a short week for most, I worked last weekend, so I’ve had a long week. ER volumes are very high throughout the area (actually nationally). While some of it is COVID related, most of it is not. Volumes declined to about 50-60% of normal early in COVID. Volumes didn’t recover until late 2021 and then dropped again early this year. However, since late April, every ER director I speak with is experiencing patient volumes much higher than pre-COVID.
ER demand is not like demand for a new iPhone. Generally speaking, people don’t like coming to the ER. Ambulance and ER utilization can be derived by population size so when we see national shifts in ER volume, we have to look at other drivers besides increases in the population (which didn’t happen overnight). During last winter’s Omicron surge, the volume was clearly driven by COVID. But that really isn’t the primary driver right now. Nationally, we’re facing challenges with workforce issues (particularly with nursing but also with physicians) and space. ER’s can’t readily expand and hospitals are full, resulting in admitted patients having prolonged waits in the ER.
Interestingly enough, in a 2017 study through the University of Maryland, it was estimated that emergency departments provided approximately 47% of all medical care delivered in the US. Over a 14 year period (that ended in 2010), there were 3.5 billion healthcare contacts made in the ER, outpatient facilities, and hospitals. Inpatient care accounted for 15% of the encounters, outpatient visits were 38%, and the rest were in the ER. While these numbers could be a touch different now, I bet they haven’t changed that much.
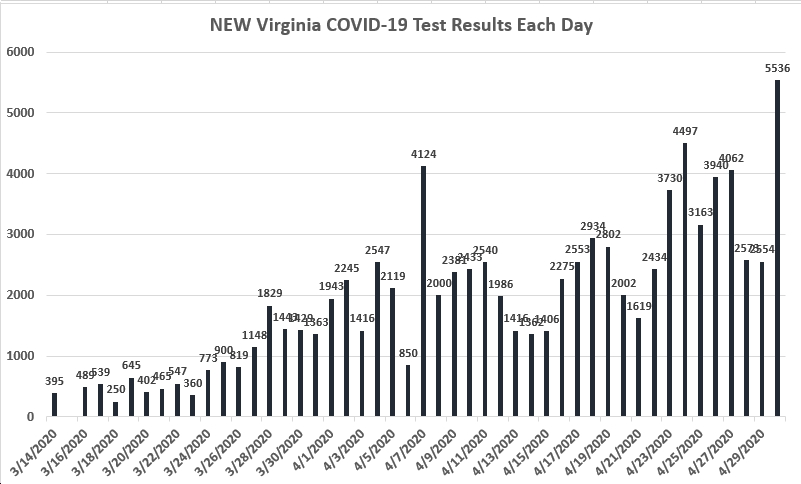
Our COVID numbers increased compared to last week, though were still lower than what we were seeing for most of July and August. Our percent positive rate of 11.7% is lower than our 6 week average of 12.2%. The number of patients hospitalized with COVID is a few more than last Friday, but in the general ballpark.
I saw an interesting tweet comparing COVID to chickenpox that said if chicken pox were a new viral disease, we wouldn’t know about shingles for another 20 years. Although we have some knowledge of the potential impact of long-COVID, we really don’t know what the impact will be in 10-20 years. Scientists are now beginning to collect data and study any potential links between long-COVID and depression with or without suicidal thoughts. Psychiatrists believe that long-COVID is associated with depression and suicidal thoughts, but they don’t have the epidemiological data to prove it. They also want to better understand if depression is caused by an inability to function at previous levels or if COVID changes the brain’s wiring. In data analysis comparing 1.3 million adults with COVID to 19,000 with long-COVID, “patients with long COVID were nearly twice as likely to receive a first-time antidepressant prescription within 90 days of their initial COVID diagnosis compared with people diagnosed with COVID alone.” We have a lot to learn about long-COVID on mental health, as well as other body systems.
The new booster is out though I think availability is tight. I haven’t gotten mine yet but will schedule an appointment soon. While lots of hospitalized patients have been vaccinated, vaccination and boosters make a difference. Published in JAMA Internal Medicine, researchers looked at 200,000 hospitalizations from January 2021 to April 2022. Although hospitalizations were always more likely in the unvaccinated group, looking specifically at the “January to April Omicron wave, hospitalization rates were 10.5 times higher in those who were unvaccinated and 2.5 times higher in those who were fully vaccinated but had not received a booster.”
Coronavirus is not done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike