Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates!
Friday Night Update from the ER in Arlington, VA
Three years ago this week, a man in Wuhan, China started feeling ill. He became the first confirmed case of COVID-19. Since then, 6.6 million people have died of COVID with 1.09 million deaths in the US.
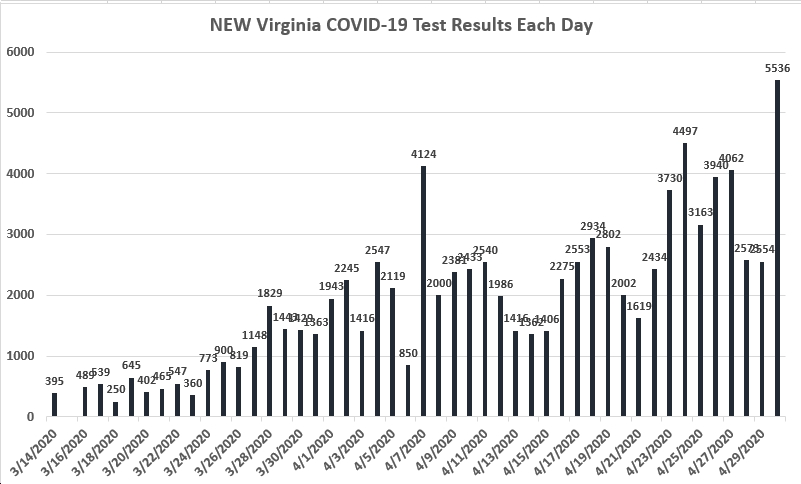
Every electronic medical record (EMR) has at least one tab referred to as the tracking board. We have a variety of these which allows each provider or nurse to view their patients, waiting patients, whole ED, etc…As a doc, I spend a lot of time looking at my board to figure out what labs are back, what I need to do next, etc…In the past, I’ve shown a screen shot of the portion of the board that is color coded for patients who have COVID test results pending versus positive or negative. Over the last month or more, it was noticeable how few positives we’d see on our board. Last week, for the first time in a while, I really felt the board had a lot more positives showing up. While we’ve been talking about flu and RSV, COVID is making a return.
We see this in our data as well. There’s been a clear increase in the number of positives among our symptomatic patients over the last few weeks. The graph looks like a staircase and we’re at the top of the stairs this past week. There’s about twice as many positives this past week versus the week before and three times as many positives as a few weeks ago. The percent positive rate has gone from about 5% to 14% in the last few weeks among this subgroup of patients.
The slope isn’t quite as pronounced among all patients tested in the ER, but we’re still seeing a lot more positives, but not quite double the positive tests this past week than previous weeks. The overall percent positivity rate also climbed from about 5-6% to 10% over the past few weeks. We’ve also seen an upward trend in the number of our COVID isolation orders used as well as a higher number of these patients being admitted. And we have more patients hospitalized with COVID now than in the last couple of months.
Flu and RSV are still around as well. We’re seeing about a 20% positivity rate on flu tests with the highest percent positivity rate among 12-17 year olds and the lowest percent positive rate in those >65 years old. Most patients get a combined COVID and flu test. I was looking at one of my lists of discharged patients earlier this week and literally a third of the patients on the list had been diagnosed with flu. However, our total numbers of positive flu tests seems to have peaked in early November with each week having a touch less. There’s still plenty to go around and we’re still seeing entire families checking in to get evaluated for flu like symptoms.
There was a great study published this week comparing regular medical masks to N95s in preventing COVID. This was an international study with 29 hospitals and over 1000 healthcare workers who provided care to COVID patients. While there were some limitations in the study design, it appears that regular masks protected healthcare workers from getting COVID as effectively as N95s.
Fellowship match occurred this week. After 4 years of college, 4 years of medical school, and 3 years of internal medicine residency, those who desire to go on for further specialty training in things like cardiology, gastroenterology, and critical care, to name a few, require a fellowship. This additional training lasts 2-6 years. After three years of a pandemic, the second lowest match rate was Infectious Disease. Over 40% of spots went unfilled. This is so unfortunate. If we’ve learned nothing else over the last few years is just how important this specialty is and how we will need these docs around in the future to deal with the next infectious disease outbreak. Why unfilled? I’m guessing it’s about money. ID docs tend to make less than other fellowship trained specialists.
And speaking of new infectious disease outbreaks, the World Health Organization has changed the name of monkeypox to mpox due to stigma and discrimination concerns. Both names are considered okay to use for the next year though monkeypox is being phased out and WHO is switching to mpox in their communication. Monkeypox was named in the 1970s, long before the WHO outlined naming best practices in 2015.
A “report published…by the CDC’s National Center for Health Statistics” found that “rates of deaths from drug overdoses among seniors have more than tripled in the past two decades.” Couple that with a “report from the National Center for Health Statistics finds that rates of alcohol-induced deaths among adults 65 and older have been climbing since 2011 and rose more than 18% from 2019 to 2020.” I can’t tell you how many times I’ve seen an intoxicated person fall and suffer a head injury. Elderly people may already have more issues with balance and stairs than when they were younger and are already at a higher fall risk. Then factor in that older patients are more likely to be on blood thinners than younger people. These meds put you at higher risk of sustaining life-threatening bleeding into your brain.
Coronavirus is not quite done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike