Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency Medicine at the Virginia Hospital Center in Arlington, for these superb updates which he posts on his Facebook page every Friday evening!
Friday Night Update from the ER in Arlington, VA
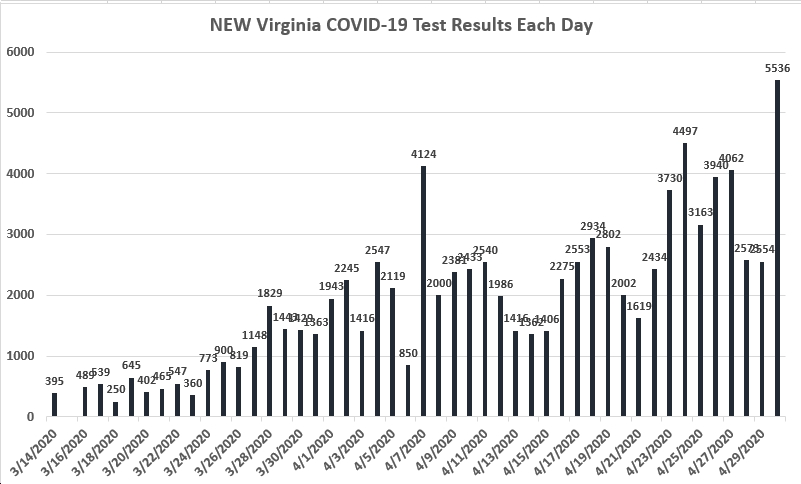
COVID numbers continue to move in the right direction. The numbers from our symptomatic patient group and all comers are both the lowest they have been since Thanksgiving. Our percent positive rate for symptomatic patients is still around 16% but was <10% in October. Overall, percent positivity is running about 10%, down from 17% the last week of the year. The number of patients we have hospitalized is down about 40% compared to last week. The CDC reported that the newest variant XBB.1.5 is now accounting for 61% of all new cases, up from 49% a week ago. Although numbers seem to be improving locally, this new variant is supposed to be more transmissible so I’m wondering if we’re see an uptick in cases.
Probably the biggest news this week on the COVID front is that President Biden “informed Congress…that he will end the twin national emergencies for addressing COVID-19 on May 11, as most of the world has returned closer to normalcy nearly three years after they were first declared.” This “move to end the national emergency and public health emergency declarations would formally restructure the federal coronavirus response to treat the virus as an endemic threat to public health that can be managed through agencies’ normal authorities.” The emergency declaration was due to expire previously and has been extended before but this does seem to be the end of it. Businesses, healthcare organizations, schools, etc…have generally returned to normal operations. COVID may never go away, and we need to continue to live with it. Certainly, mortality rates have decreased dramatically over the last three years (though 500 people a day are still dying of COVID) and hospitalizations are also down. I’m not sure I understand all the ins and outs of this of the President’s move, but it seems like the biggest impact will be the government transferring the responsibility for payment of vaccines and some treatments to insurance companies and individuals. Like many things in healthcare, the poor and/or underinsured will be impacted more than others. It’s estimated that about 17% of Medicaid enrollees will lose coverage. If you don’t have insurance, getting vaccines and meds like Paxlovid may end up prohibitively expensive, leading to an exacerbation of health inequity.
Hybrid immunity refers to those who have immunity due to a combination of having received the COVID vaccine and also having had COVID. Given that the majority of the country has been vaccinated and also has had COVID, scientists sought to answer the question as to how effective hybrid immunity is via a systematic review and metaregression. This could have implications for determining vaccine frequency. Findings showed that “people who are vaccinated and have previously been infected with COVID-19 had a 97% reduced chance of severe COVID-19 infection 1 year after their last vaccination or infection.” Effectiveness against reinfection with hybrid immunity was estimated at 41% at 12 months.
Through my involvement with the state chapter of the American College of Emergency Physicians, I was at a legislative reception last week. This was our chance to bring our concerns as emergency physicians to state legislatures. We typically talk about psychiatric patients and how difficult it is to find beds for patients who need inpatient care and ED overcrowding issues. One of the more animated conversations this year had to do with drug testing which then ultimately led to a conversation about Narcan distribution. Ideally, if a patient has an opioid overdose and ends up in the ER, they would leave with a dose of Narcan, not just a prescription for it. There’s a variety of barriers to getting this done.
Narcan can be a life saving drug for someone who overdoses on opioids. By nature, opioids cause sedation, but they can also cause depression of the respiratory system and make you stop breathing. If you stop breathing long enough, your heart will stop as well. If you work in Northern Virginia, you likely heard about the apparent drug overdose at Wakefield High School. I’m getting my details from Arlington Now. It sounds like the student was found unresponsive in the bathroom, was brought to the hospital in critical condition, and died yesterday. The case is every parent’s worst nightmare. I want to talk about opioid overdoses and Narcan (naloxone).
Probably the biggest fear I have is that one of my kids gets offered a pill at a party by a friend who says “try this.” I guess my real biggest fear is that my kid says “thanks” and actually takes it. While I don’t think they would, it’s something I regularly talk to my high school son about. Fentanyl is so prevalent and so dangerous, and there’s not a lot of quality control being done with street drugs. What a kid thinks might be an oxycodone (which shouldn’t kill an adult sized high school student), could have fentanyl mixed in, which could cause an adult sized high school student to become unconscious, stop breathing, and die.
Narcan can reverse this. It blocks receptors in the brain that opioids are trying to bind to. I’ve seen many patients who overdosed on opioids, generally heroin, who were unresponsive and not breathing, literally minutes away from dying and some even get CPR, who get Narcan, start to breath on their own, and generally, pretty quickly, get back to their baseline mental status. In the ER, we’ll generally observe routine overdose patients for a while, as the Narcan may wear off before the opioid does and the patient can become symptomatic again. There are also risks of other complications that can occur with drug use/overdoses that we’re monitoring for.
Narcan is safe to give and is commonly used by EMS for unresponsive patients. Afterall, it potentially reverses a life-threatening event and can take an overdosed unresponsive, non-breathing patient and bring them back to life. I don’t keep Narcan at home or in the car but if I was tempted to give it, it would have to be in parallel with calling 911 and possible starting CPR. Narcan only works to block opioids, so it won’t interfere with other medications.
Narcan is indicated for the patient suspected of having an opioid overdose, with signs of breathing difficulty or excessive sleepiness. Opioids slow down your breathing rate and can stop breathing. An unresponsive student in a school bathroom is certainly likely to be an overdose. There are of course other things that could cause a student to be unresponsive. Post ictal after a seizure is one possibility. Hypoglycemia is a frequent cause of unresponsiveness, as well, which is why EMS will either check a glucose level or give IV D50 (sugar) to unresponsive patients as well. Much less likely, but not impossible, would be some that causes bleeding around the brain (trauma, ruptured aneurysm).
Years ago, I had a young adult come into the ER with an asthma exacerbation. She was very sleepy. Asthma and sleepiness can mean impending respiratory failure. I also thought she might be high on heroin and specifically asked her this. She denied any drug use. I decided to give her a dose of Narcan. I was an intern and hadn’t quite mastered the dosing of Narcan, but I followed the book and gave a full 2 mg dose. Wow, what a response. She woke up. She also was in florid opioid withdrawal, complete with yelling, vomiting, and sweats. And anger. I learned that I could have given a smaller dose to achieve the desired result of increasing breathing and confirming that the sleepiness was related to drugs and not asthma. With that said, if I was not in an ER, and was going to give Narcan to my unresponsive kid that I thought was a result of an OD, I would give the fill dose.
Facebook memories were good to me today. First, there were no COVID related posts that popped up as memories. It’s nice to know that we had lives before COVID, and I remain optimistic that we’ll return to a time when COVID isn’t such a prevalent part of healthcare workers days. Better though, was today marks the 10 year anniversary of the Raven’s winning the Super Bowl. My wife and I were lucky enough to go in what turned out to be a 21 hour round trip to New Orleans. What a game, complete with a black out, and what a road trip.
Coronavirus is not quite done with us yet.
Science matters. Get vaccinated (or your booster). Keep a mask handy.
Mike