Great Facebook post by Dr. Mike Silverman, Chair, Department of Emergency medicine at Virginia Hospital Center
Friday Night Update from the ER in Arlington, VA
The CDC Director Dr. Rachelle Walensky announced this week that the delta variant makes up more than 82% of the new cases that are sequenced. This has grown from less than 10% about a five weeks ago. Delta will be the dominant variant until the next variant that is more transmissible than delta takes hold. This is inevitable as it’s the way mutations work. I heard on the news the other day that there have been 60 cases of Delta in the state of Maryland. What’s important to recognize is that this number is based on sequencing and proving that the positive Covid test was a result of the Delta variant, not the total number of people in the state who have been infected by the Delta variant. Only a very small percentage of all positive cases are sent for sequencing. There are certainly more than 60 patients in Maryland who are carrying the Delta variant.
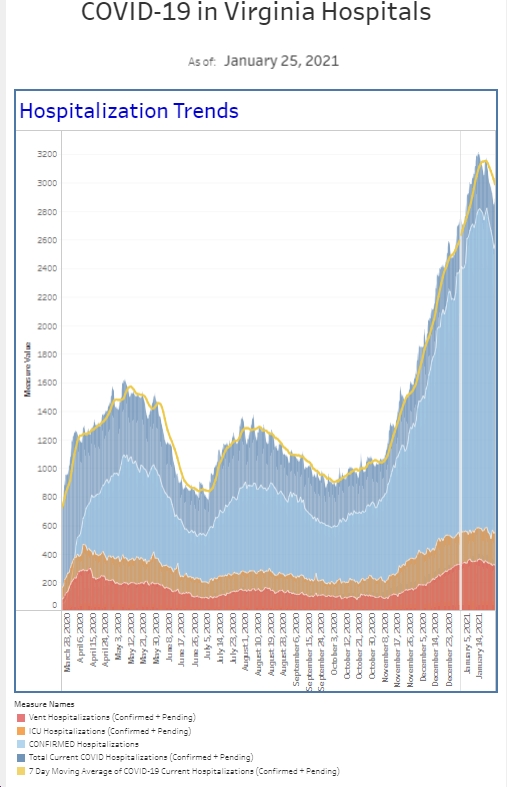
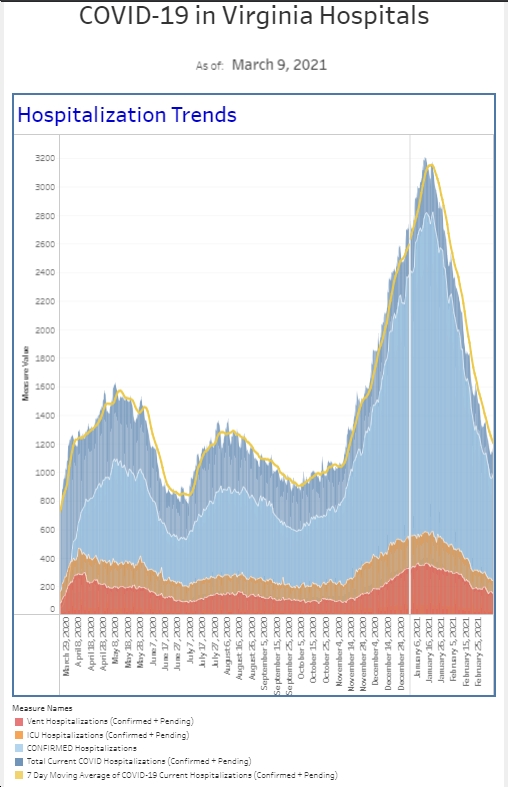
When I wrote last week, we had our first real uptick in the amount of positive cases requiring hospitalization. The number of patients admitted to the hospital is about double what it was this time last week. Although that number is still relatively small compared to how many patients we were managing during the winter surge, it’s certainly a number worth following for now. As I was working this week, one of my colleagues said to me, “Wow, it definitely seems like COVID is back.” Whereas a couple weeks ago, I probably had not seen a Covid patient in several weeks, this week, I had several. Our actual number of new diagnoses based on our testing this week, is a touch lower than the previous week and our overall percent positive rate among emergency department patients is actually down a touch from the previous week as well. However, it is 2-3 times higher than it was in the month before that. However, we are seeing patients come in after having positive tests as outpatients and then requiring further intervention. I have not talked a lot recently about the number of patients who require our Covid “enhanced isolation” protocol recently. We have been tracking this since the very beginning and I have talked about it during surges and at the end of surges the numbers have gotten flat. Patients that we believe potentially could have Covid are placed in the special isolation category. These numbers have been flat since about mid-June. We saw this number increase about 20% the second week of July and then this past week it increased another 20%. On the hospital side, after previously pausing our COVID task force meetings, we have them back on the calendar. Clearly, COVID is not done with us yet.
I have attached to pictures. One is a chest x-ray of a young adult patient with a fairly severe Covid pneumonia. This patient had refused vaccination though was certainly interested in being vaccinated once he realized how hard it was to breathe with Covid pneumonia. The second picture is me. My surgical mask is over my N95. Although I had not been routinely wearing my N95 for my entire shift the last several weeks, I reversed course last weekend when I worked and decided I needed to be in an N95 for the entire shift.
The number of new positive cases have increased across the country. Although ER and hospital admissions are up, we really see the bump in those patients a couple of weeks after case numbers increase. My daughter pointed out to me today the number of her friends and contacts, all vaccinated, who have become sick and tested positive. It’s a bigger number than I would have expected. She also pointed out that this group isn’t coming to the ER. As I’ve said before, we start to get busy after community spread has a time to infect older and medically compromised people.
Just a little vaccine news. In a pre-print study, (so not peer reviewed yet), the NY Times is reporting, that the J&J vaccine might be “much less effective against the Delta and Lambda variants than against the original virus.” Results show the vaccine “consistent with observations {with} a single dose of the AstraZeneca vaccine – which has a similar architecture to the J.&J. vaccine – shows only about 33 percent efficacy against symptomatic disease caused by the Delta variant.” We’ve already been talking about patients who received a J&J vaccine getting a booster. Although the science hasn’t supported that yet, I suspect the science will continue to evolve, so don’t be surprised if ultimately it’s recommended that J&J vaccine recipients get boosters before those of us who got Pfizer or Moderna. On the positive side, the CDC’s Advisory Committee on Immunization Practices (ACIP) has posted data ahead of today’s meeting regarding the Guillain Barre Syndrome cases around J&J administration and believe that the benefits of vaccine outweigh the risk of GBS and :strongly support” it’s continued use.
The American Hospital Association represents 5000 hospitals and healthcare systems. They released a statement this week saying they support mandatory vaccination for hospital employees. AHA CEO Rick Pollack said in prepared remarks. “The AHA supports hospitals and health systems that choose, based on local factors, to mandate COVID-19 vaccines for their workforce. Doing so will help protect the health and well-being of healthcare personnel and the patients and communities they proudly serve.” This week, NYC announced that city run healthcare facilities and hospitals will require either vaccination or weekly testing for the unvaccinated healthcare worker. As I said last week, my sense is that it will be much easier to mandate once the vaccine is given full FDA approval. I hope that happens soon.
For those wondering, I’m generally back in a mask when I’m indoors at a store. The vaccine is doing a great job of protecting people from hospitalization and death, and I really want to avoid getting sick as I can’t take the time away from work. Wearing a mask seems like an easy way to help myself.
Science matters. Get vaccinated. Wear a mask when you’re supposed to. We’re almost there.
Mike