Great update by Dr. Mike Silverman, Chair, Department of Emergency medicine at Virginia Hospital Center. For last Friday night’s update, see here.
Friday Night Update from the ER in Arlington, VA
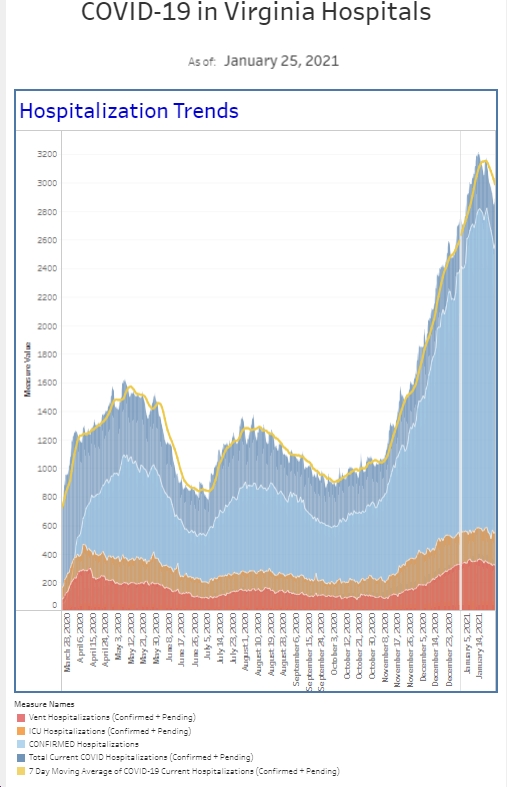
This is a pretty data heavy post. But let’s start with what’s in the ER. We continue to see a slight uptick in COVID diagnoses that we are making in the ER. Cases are certainly climbing across the country and even locally in the DMV. Fortunately, we’ve not seen a surge in the ER yet, but numbers of new cases weekly continue to trend upwards with this past week seeing our highest number in many weeks. Our percent positive rate is also trending up. One interesting twist I noticed was when I did some telemedicine work this week. About half of my patients had signs and symptoms of COVID and I recommended testing. Over the last few months, it’s been very unusual for me to have any telemedicine patient where I was worried about COVID.
Although our hospitalization numbers are similar to last week, we’re seeing an increase in the admission rate (the percent of patients admitted versus discharged) among our COVID isolation patient subgroup. We’re also seeing our highest positivity test rate among our symptomatic patients and among all comers to the emergency department since early May.
I spent a lot of time talking to vaccine hesitant patients, family members, and acquaintances over the last week or so. With 190 million doses given in the US, it’s certainly hard to call the vaccine experimental. People have all kinds of reasons why they are reluctant to get a vaccine. Much of it is a lack of understanding of the science (it doesn’t change your DNA), the long-term effects (there’s no data to suggest it impacts fertility), and that it was not “rushed.” In fact, the vaccine was 20 years of science in the making and getting the EUA shows what happens when you have a lot of community spread (you need enough people to get sick to show differences in the two groups) and perhaps reduce the red tape to get it reviewed. There were no differences in the safety and efficacy standards required versus any other vaccine. And while previously having COVID offers a layer of protection, receiving the vaccine afterwards remarkably increases your immune response and makes you safer.
Masks and Vaccine information continues to dominate the news that I am getting.
The CDC provided an updated recommendation on mask use. Although they seem to have changed course, they said it’s in response to the increased transmissibility of the Delta variant. And you know what, it makes sense. The Delta variant not only has increased transmission rates, it also leads to higher viral loads in vaccinated patients making it easier for asymptomatic vaccinated patients to infect people. Here’s what the CDC said: masks should be used in school (K-12). They also recommended mask use in areas with “substantial” or “high” COVID rates defined as more than 50 (substantial)-100 (high) new cases/100,000 population as a 7 day average. You can find your local area numbers online. Alexandria, DC, and other local areas are at or above the 50/100K number currently. In these areas, even if you’re vaccinated, you should use a mask in public indoor spaces, and crowded outdoor areas. Recall, unvaccinated people were recommended to do that anyway, but we all know that once mask mandates went away, almost everyone stopped wearing masks regardless of vaccination status. Like I said last week, although most indoor activities I’ve doing are not in areas with “substantial or high” rates, I’m back to wearing a mask when I’m in public indoor spaces. Masks will protect you from others and will protect others from you.
Last Friday, after I finished writing my post, there were preliminary reports out of Israel based on a small sample though during a high delta variant, that suggested that the 2 shot Pfizer vaccine was only 39% effective at reducing the risk of infection and 40% effective at reducing the risk of symptomatic disease. The vaccine was greater than 90% effective at preventing severe illness. However, a new study out of the UK that was published in the New England Journal this week found the vaccine to be 88% effective in preventing symptomatic COVID. This is obviously a large discrepancy and scientists are trying to account for the differences. One of the questions is whether immunity fades over time and how quickly that happens. Certainly, the good news is that in both studies the vaccine appeared effective in reducing serious illness and death. And that is the perhaps the most important reason to get vaccinated.
On Wednesday, Pfizer released internal data via their 2nd Quarter Earnings Teleconference (you can easily find the slides online) and a pre-print paper that a 3rd dose of the vaccine can “strongly” boost protection against the Delta variant, with up to a fivefold increase in antibodies for people 18-55 and an 11 fold increase for those 65-85. Before you ask, they did not post data on the 56-64 year old age group. They estimate the potential for up to 100 fold increase in Delta neutralization after the third dose, which certainly sounds good. This is a small study, measuring antibody levels of 23 patients and we really don’t know if that level of protection is even needed. In the same pre-print paper, they said that overall efficacy of the vaccine was 91%, down from it’s peak of 96% 1-2 months after the second dose. Ultimately, at 6 months, Pfizer estimates efficacy around 84% (most healthcare personnel are now 7+ months out from their second shot). Pfizer is estimating that efficacy declines about 6% every two months, so it does seem likely that we’ll have a booster shot sooner rather than later. Overall, at 6 months, it’s about 97% effective against severe disease. Of their initial 44,000 volunteers, I’m hoping they did a formalized blinded, placebo controlled study with a 3rd dose on at least half of them as then we’d have a better sense of the efficacy comparing 2 to 3 doses. I’ve heard they were studying the third dose but I don’t know the details, though Pfizer has said it plans on submitting data regarding the 3rd dose within the next month. (I have no doubt Moderna is conducting similar studies but remember, Moderna was approved a few weeks after Pfizer, and they have reported data a bit after Pfizer reports data). Ultimately, it will be up to the FDA and CDC about whether a 3rd dose is indicated. Right now, the official word is we don’t need it. A couple of other interesting points from the Pfizer slides are: they do expect boosters to start with immuncompromised (see next paragraph) and older adults, they expect review of the vaccine for full FDA approval in January 2022, and they have manufactured an mRNA vaccine specific to the Delta variant with clinical studies projected to begin in August.
Researchers also published the benefits of a booster shot for kidney transplant patients, published in a JAMA research letter. In the population studied, they were able to identify subgroups that showed more benefit than others. Transplant patients are immunosuppressed and this may serve as a model for others. Israel started giving booster shots to patients >60 years old this week as well. If vaccinated healthcare workers start to get sick in the near future, I’d expect a bigger push for boosters. After all, we are the canaries in the coal mine. Fortunately, reported in the NEJM this week, among 1497 fully vaccinated healthcare workers, the breakthrough rate was 2.6%, with mostly mild symptoms or patients being asymptomatic. However, 74% of cases had a high viral load. The good news, breakthrough cases were uncommon with generally mild symptoms. However, the high viral load shows the potential to spread disease. As I said before, I have no doubt that boosters are coming. The question is who they will be recommended for first and what will the timing be.
Another interesting study out of the UK looked at the timing of the second dose of the Pfizer vaccine. In order to vaccinate more people, the UK initially was recommending receiving the second dose 12 weeks after the first. In a preprint not yet peer-reviewed study, researchers looked at the immune responses of over 500 hospital staff who received their 2 shots at different intervals. They had some interesting findings. First, regardless of when you received your second shot, all people had a strong immune response. Researchers believe that the ideal second dose may occur around the 8-week mark, which allows for a higher proportion of helper T cells, which helps with immune memory. The interval difference of the second shot between the UK and Israel may help explain some of the differences in the efficacy studies I mentioned a few paragraphs earlier. Another potential explanation is that the Israeli study included people who were farther out from their second shot than the UK study.
The picture shows a column from our EMR tracking board. Early in the pandemic, we added a column for COVID test results so ER docs had results in our face as we worked on the computer.
Science matters. Get vaccinated. Wear a mask when you’re supposed to. We’re almost there.
Mike