Thanks as always to Dr. Mike Silverman, Chair of the Department of Emergency medicine at Virginia Hospital Center, for these helpful updates!
Friday Night Update from the ER in Arlington, VA
First off, we are diagnosing a lot of COVID in the emergency department. Patients classified as being symptomatic are testing at a 64% positivity rate. That is up from 59% last week. The good news is we had less symptomatic patients this week than during the holiday week and an overall decline of about 20% of new positive cases among this group of people. It is really crazy to look at the graph that I have kept throughout the pandemic because the number of new cases we’re diagnosing is on a whole different scale than previous surges. We’re seeing 5 times more positive cases among our symptomatic patients that in either of the previous surges. We’re also doing a considerable amount of testing on patients that are classified as asymptomatic. As a reminder, these are patients generally being admitted to the hospital for non-COVID related reasons or have symptoms that are not consistent with COVID. The positivity rate among these patients was less than 1% last week of November. This week, it was over 29%, up from 24% the week previous.
Many of my asymptomatic patients who have tested positive have presented with headaches, primary psychiatric issues, or were asymptomatic but had a known exposure and required a test prior to admission. Admitted patients who have COVID as a secondary diagnosis still present risk to the staff and require additional time for donning and doffing PPE. Adult patients considered asymptomatic are often brought to the ER for weakness or confusion, so not the classic symptoms such as fever, cough, or shortness of breath. Yet, we’re finding they require admission for altered mental status, acute kidney injury, or metabolic derangements, such as very elevated glucose levels or very low sodium levels.
As some people have argued, the absolute number of positive cases may not matter in the grand scheme of things. It is the number of hospital admissions and deaths that matter the most. On the other hand, these relatively healthy asymptomatic patients do increase the risk of others getting sick. And hospital volumes are maxing out because of the large numbers of COVID patients hospitalized. When we look at all comers this past week, again we saw an increase in the overall positivity rate. About 43% of all COVID tests we run are coming back positive. Even during our first surge in the spring 2020, that number was only about 20%. It was also about 20% a year ago during last winter’s surge. We did test less patients this week than last week, and had less overall new positive cases. While I hope this trend continues, the snow day Monday had a significant impact on the number of patients that we saw over 24-hours, and I suspect that had we seen our normal volume, the story might be a little bit different.
The week between Christmas and New Year’s was the highest patient volume week we have ever had in the emergency department. We were about 30% above baseline volume. Excluding the snow day which impacted this week’s volume, average volume is still higher than typical. The next week will certainly be telling as kids go back to school and everyone gets out of the holiday mode. I personally know a lot of people who got COVID over the holidays and I expect to see cases continue to grow for the next couple of weeks.
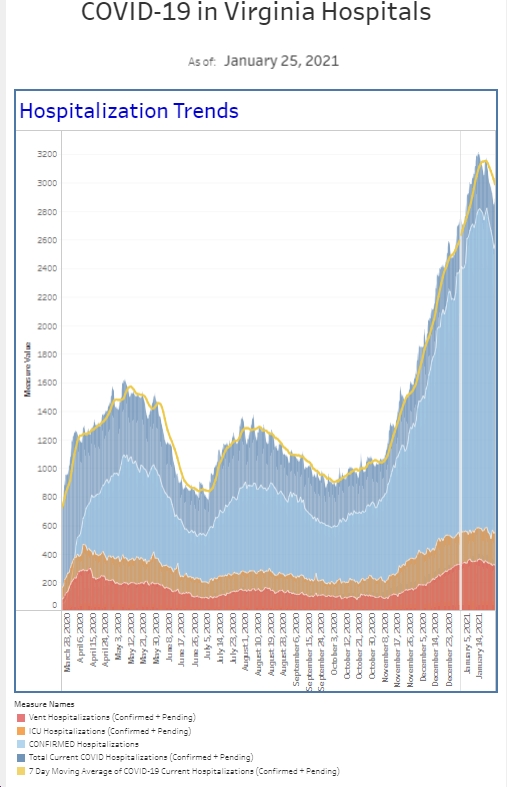
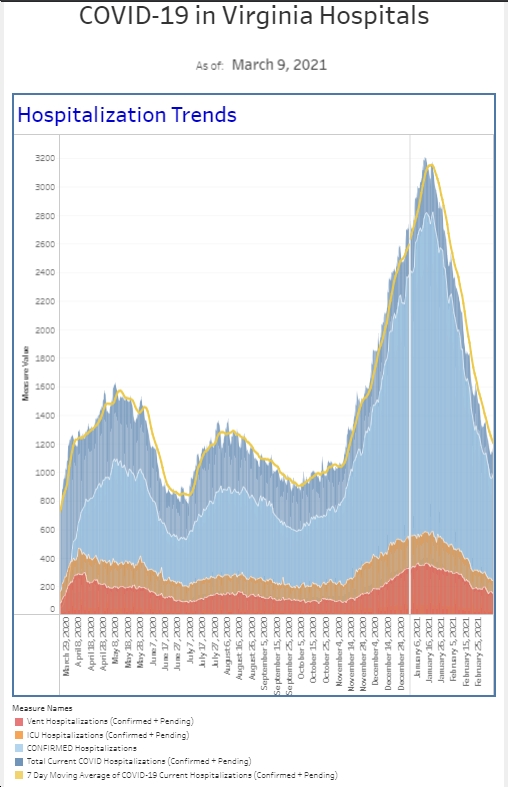
The hospital has set a new record for the number of COVID inpatients we currently have hospitalized. That’s not the kind of record anyone wants to break. We’re up about 50% compared to last week. Unlike other surges, the hospital, like all other hospitals, is also strained by non-COVID patients. On the plus side, the ICU is telling me that they’re seeing much more success getting people off ventilators now than during the Delta surge.
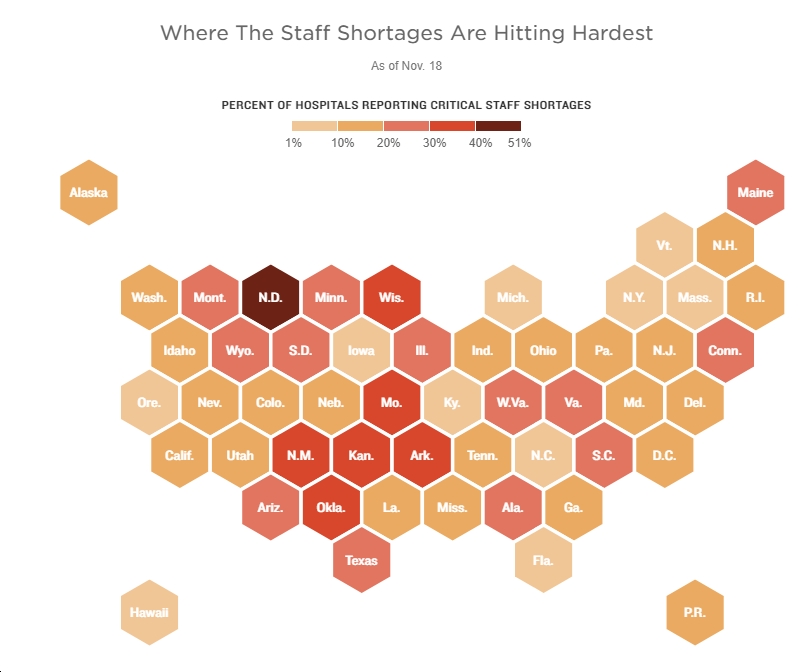
Let’s switch gears and talk about the CDC isolation criteria. A couple of weeks ago I wrote that my biggest concern was whether we would have enough healthcare workers to staff the ER, the hospital, offices, etc. Most of us work through mild illness and given the choice, if we were asymptomatic, most of us would rather work than have a 10-day furlough. As airlines were canceling flights because they did not have enough staff and hospitals, EMS, and police agencies were also experiencing staff shortages, the CDC came out with new criteria that allows people to return to work after 5 days while wearing a mask for an additional 5 days. Without getting into all the details, for the vaccinated, boostered, asymptomatic healthy person who work in a critical industry, this may make sense. However, since the average person sheds virus for 7-10 days, this probably does not make sense for society as a whole. Particularly true when considering mask compliance across the country, which is necessary for days 6-10.
The rapid antigen test may make sense when clearing people to return if inside of 10 days, but the studies aren’t completely clear. Now I realize, you probably cannot get any at your local drugstore. I ordered 1 per family member on Amazon this week just so I can have some down the line if/when someone becomes symptomatic.. But assuming we had access to over-the-counter antigen test, a negative test means you are most likely not shedding virus and it would be safe to stop isolating. Much like the NFL requires 2 negative tests 24 hours apart (they’re using PCR tests not antigen), a negative antigen testing strategy makes sense to me to stop isolating.
I talked to the father of a patient recently who said his child required a negative PCR test to return to school. I diagnosed the child with COVID earlier this week and had called to check on my patient’s status. The problem with the PCR test is that it can be positive well after the CDC recommended 10 days of isolation. The PCR test can pick up dead mRNA and result in a positive test even though you are actively not shedding virus. Hospitals typically are not testing employees to return to work but rather letting them return after 10 days. Given how hard it is to schedule a PCR test, I hope school systems and employers will find an alternative strategy to allow people to return safely to the classroom and work environment.
Related to this, kudos to Maryland’s governor for opening mass testing centers that do not require an appointment. These centers will do rapid antigen tests so that positive people can immediately isolate while also sending out PCR tests and then sending results via text 1-2 days later.
There should be a lot of relieved parents this week as the FDA and CDC approved booster shots for the 12-15 year old crowd. The other big change was recommending boosters 5 months after the second dose of vaccine instead of 6, and recommending a 3rd shot 28 days after the second dose for the immune compromised, including kids 5-11. While there’s still work to be done for pediatric vaccinations, these boosters will make schools and kids safer.
We’re certainly seeing a lot of COVID positive kids. We’ve transferred several critically ill kids to pediatric intensive care units (PICU) and this includes kids ranging from newborns to upwards of 12 years old, both vaccinated and unvaccinated (obviously those <5 are unvax). One of the more interesting things we’ve seen are the number of kids who have croup secondary to COVID. Croup is inflammation of the upper airway, typically caused by a virus, and usually results in a barking, seal like cough. We see it commonly in the ER and we typically can get kids improved and home in a matter of hours. However, we’ve had several really sick kids from croup who required a PICU bed. Please get your kids vaccinated and boosted if they qualify. It will make a difference.
The CDC revised the Omicron numbers again. The week ending on Christmas had been reported at 59% and that number has now been revised to 77%. And for last week, the number is 95% Omicron (estimated to be 93% in NoVa). Data always must pass the sniff test and these numbers are consistent with what we’re seeing clinically—ease of spread (our numbers spiked the week before Christmas), milder symptoms, extreme fatigue, less loss of taste and smell, chest and abdominal pain, headaches, and a lot more croup in pediatric patients. These presentations are different than what we’d seen previously. In my world, I don’t know what variant you have and can’t test for it. I make the clinical decision about whether or not you need hospitalization. Only one of the available Monoclonal antibodies has effectiveness against Omicron and MAB are in such short supply, it’s unlikely that you can get them.
There was an article published by the CDC this week looking at the percent of vaccinated patients who ended up with hospitalization or death. Data was obtained through a large US healthcare database containing 465 hospitals and included more than 1.2 million patients. The authors found that severe COVID and death were very rare, occurring in 0.015% and 0.0033% of patients respectively. They also found that all patients with severe outcomes had at least one risk factor that made them high risk and that 78% of those who died at least four risk factors. While the rates seem low to what we would guess is going on, I admit that my ER view is somewhat biased as I don’t see all the patients who are not coming to the ER. With that said, the benefit of understanding these risks means older, high-risk patients need to continue to protect themselves from exposure to COVID while the healthcare system can also prioritize them for pharmaceutical intervention (including MABs when they’re available).
There are new treatments becoming available, including the Pfizer oral medication and another outpatient infusion. More on those in the near future.
If you don’t have a pulse ox yet, please buy one online. $25 will get you a pretty good one. If you get sick, it’s really important to know what your oxygen is when you’re sitting and when you’re walking (just normal pace like you’re walking to the bathroom). A doctor’s decision to admit you may come down to something as simple as what your walking pulse ox level is and certainly if yours is less than 93%, you should come to the hospital to get checked out.
The Coronavirus is not done with us yet.
Science matters. Practice physical distancing. Get vaccinated (or your booster). Wear a mask.
Mike
PS The picture this week is from today’s noon medical staff webex update. Seated in the room from left to right are the directors of the hospitalist group, ER (me), infectious disease, and ICU and our chief medical officer. We did these live webex “radio talk show style” updates regularly for the first year of the pandemic but haven’t needed them in a while. It’s a sign of the times.